What Is Metastatic Cancer, Diagnosis, and Treatment
Hearing the words “stage four” or “metastatic cancer” can feel like the ground has fallen away. While a diagnosis of cancer that has spread from its original site is serious and changes the treatment landscape, it is not a uniform prognosis. Today, with significant advances in systemic therapies, imaging, and supportive care, many people live well for years with metastatic disease, managing it as a chronic condition. Understanding what metastasis means, how it is treated, and what resources are available is the first step in regaining a sense of control and navigating the path forward.
Defining Metastatic Cancer
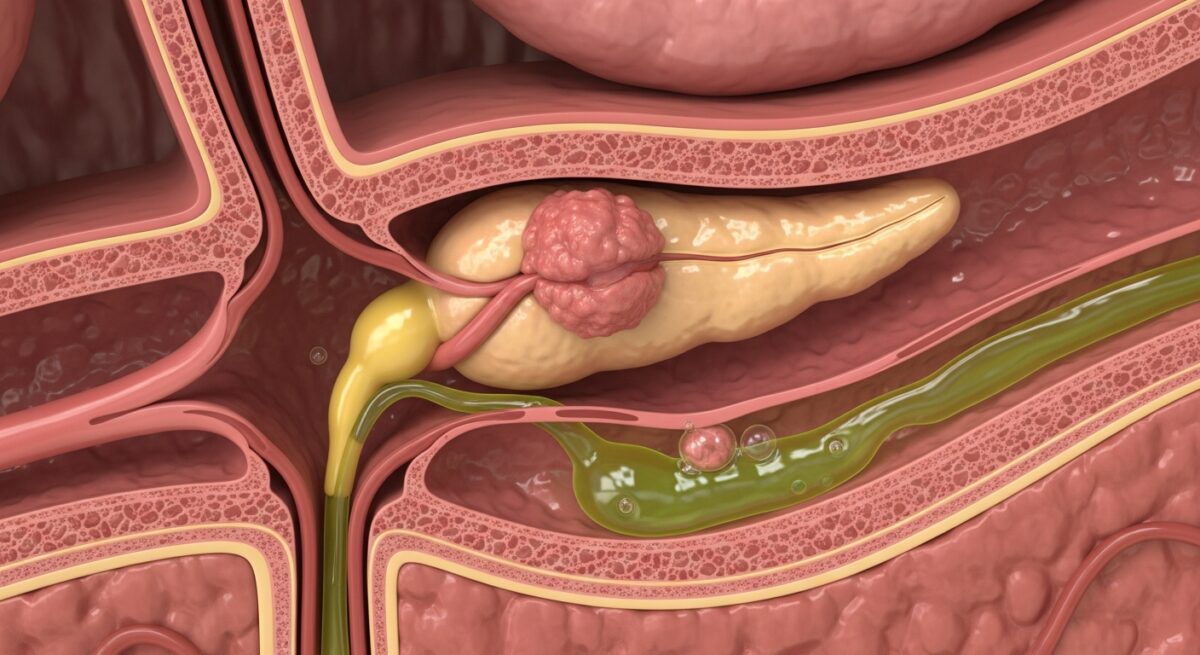
Metastatic cancer, also called stage IV cancer, occurs when cancer cells break away from the primary tumor, travel through the bloodstream or lymphatic system, and form new tumors in other parts of the body. This process is called metastasis. It is crucial to understand that metastatic cancer is named for the original, or primary, cancer site. For example, if breast cancer spreads to the bones, it is called metastatic breast cancer, not bone cancer. This distinction is vital because the treatment is based on the primary cancer’s characteristics, not the organ where it has spread.
The most common sites for cancer metastasis are the bones, liver, and lungs, though different cancer types have specific patterns of spread. The biology of metastasis is complex, involving cancer cells evading the immune system, surviving in circulation, and adapting to a new organ’s microenvironment. While metastasis signifies advanced disease, the outlook varies dramatically based on the cancer type, available treatments, genetic markers of the tumor, and the individual’s overall health. It marks a shift from curative intent, often possible in early-stage cancers, to a focus on controlling growth, relieving symptoms, and prolonging quality of life.
How Metastatic Cancer Is Diagnosed and Staged
The diagnosis of metastasis often begins when a patient experiences new symptoms, such as persistent bone pain, unexplained weight loss, or neurological changes. Sometimes, it is discovered during routine surveillance scans for a patient with a history of early-stage cancer. The diagnostic process involves a combination of imaging tests, biopsies, and laboratory analyses to confirm the presence of metastatic disease and characterize it.
Imaging tests are the cornerstone for locating metastases. These may include computed tomography (CT) scans, magnetic resonance imaging (MRI), positron emission tomography (PET) scans, and bone scans. Each modality offers different information: CT scans provide detailed cross-sectional images of the body, MRI is excellent for visualizing the brain and spinal cord, and PET scans can detect areas of high metabolic activity typical of cancer cells. Once a suspicious area is identified, a biopsy may be performed. A biopsy involves taking a small sample of tissue from the metastatic site, not just the primary tumor. Analyzing this tissue confirms the diagnosis and, critically, allows for modern molecular testing.
This molecular profiling is a game-changer in metastatic cancer care. Tests can identify specific genetic mutations, proteins, or other biomarkers within the cancer cells. For instance, a biopsy of metastatic lung cancer might be tested for mutations in the EGFR or ALK genes, which can be targeted with highly effective pill-based therapies. Similarly, metastatic breast cancer tumors are tested for hormone receptors (ER/PR) and the HER2 protein. This information moves treatment beyond a one-size-fits-all approach to a personalized strategy. Staging for metastatic cancer is consistently stage IV, but the detailed diagnostic report, including the sites of spread and biomarker profile, creates the nuanced roadmap for treatment decisions.
Treatment Strategies and Goals of Care
The primary goals of treating metastatic cancer are to slow or stop the growth of the cancer, shrink tumors to alleviate symptoms, improve quality of life, and, when possible, extend survival. Treatment is almost always systemic, meaning it travels throughout the body to reach cancer cells wherever they may be. The choice of therapy depends heavily on the type of primary cancer, its biomarker profile, the extent and location of metastases, the patient’s prior treatments, and their overall health and preferences.
A multidisciplinary team, including medical oncologists, radiation oncologists, surgeons, palliative care specialists, and nurses, collaborates to create an integrated plan. The main categories of systemic treatment include chemotherapy, hormone therapy, targeted therapy, and immunotherapy. Chemotherapy uses drugs to kill rapidly dividing cells and is a workhorse for many cancers. Hormone therapy blocks hormones that fuel certain cancers, like breast and prostate cancer. Targeted therapy uses drugs designed to attack specific molecular vulnerabilities identified in the tumor’s biomarker testing. Immunotherapy helps the patient’s own immune system recognize and destroy cancer cells.
Local treatments, such as radiation therapy or surgery, are still used in the metastatic setting but for specific purposes. Radiation is excellent for treating a painful bone metastasis or relieving pressure from a brain tumor. Surgery might be used to stabilize a bone at risk of breaking or to remove a single, isolated metastasis (a procedure sometimes called “oligometastasectomy”). A crucial component of modern metastatic cancer care is early integration of palliative or supportive care. This specialty focuses on managing pain, nausea, fatigue, and emotional distress, and it has been shown to improve both quality of life and, in some cases, survival outcomes. It is appropriate at any stage and works alongside cancer-directed treatments.
Navigating Insurance and Medicare Coverage
Managing the financial aspects of metastatic cancer treatment is a significant concern. Treatments are expensive, and coverage can be complex. For individuals aged 65 and older, or those with certain disabilities, Medicare is a primary source of health insurance. Understanding what Medicare covers is essential. Original Medicare (Part A and Part B) covers inpatient hospital care, doctor visits, diagnostic tests, and outpatient chemotherapy administered in a clinic. However, it does not cover prescription drugs taken at home, which includes many modern targeted therapies and immunotherapies. For that, a separate Medicare Part D prescription drug plan is required.
Many beneficiaries choose a Medicare Advantage (Part C) plan offered by private insurers. These plans bundle Part A, Part B, and usually Part D, and often include extra benefits like vision, dental, and fitness programs. However, they typically have provider networks and require plan approval for certain services. When dealing with a complex condition like metastatic cancer, it is critical to verify that your cancer center and specialists are in-network for an Advantage plan. The rules for prior authorizations and step therapy (trying lower-cost drugs first) can also impact access to specific treatments. For more detailed guidance on navigating these plans during serious illness, Read full article provides additional details.
Key considerations for insurance navigation include reviewing your plan’s summary of benefits, understanding your out-of-pocket maximum, investigating whether you qualify for Extra Help with Part D costs, and consulting with a hospital financial counselor or social worker. They can help with applications for patient assistance programs run by pharmaceutical companies or non-profit organizations that may help cover copays or provide drugs at low or no cost.
Living With Metastatic Cancer
A diagnosis of metastatic cancer initiates a continuous journey of treatment and adaptation. Living well involves more than medical appointments, it encompasses physical, emotional, and practical dimensions. Building a strong support system is paramount. This includes not only family and friends but also connecting with others who have metastatic disease through support groups, either in-person or online. These communities provide unique understanding and practical advice.
Managing side effects proactively with your care team is essential for maintaining quality of life. Nutrition also plays a key role; many cancer centers have dietitians who specialize in oncology to help manage weight loss, muscle wasting, and treatment-related food aversions. Gentle exercise, as tolerated, can combat fatigue, improve mood, and maintain strength. Furthermore, addressing mental health through counseling or therapy is highly recommended to manage the anxiety, uncertainty, and grief that can accompany this diagnosis. Practical planning, such as discussing advance directives and financial matters, can also provide peace of mind and ensure a patient’s wishes are known.
Frequently Asked Questions
Is metastatic cancer always terminal?
While metastatic cancer is currently considered incurable for most solid tumors, it is not immediately terminal. Many people live for years with controlled metastatic disease, thanks to evolving treatments. It is increasingly viewed as a chronic illness that requires long-term management.
What is the difference between metastatic and advanced cancer?
The terms are often used interchangeably, but “advanced” can sometimes include locally advanced cancers that have spread extensively in the original area but not to distant organs. “Metastatic” specifically means the cancer has spread to distant organs or lymph nodes.
Why do I need another biopsy if I already know I have cancer?
A biopsy of a metastatic site is critical for two reasons: to confirm the spread is from the original cancer and not a new primary cancer, and to perform updated biomarker testing. The genetic profile of cancer can change over time, and the new biopsy can reveal targets for new therapies.
Can metastatic cancer go into remission?
Yes. With effective treatment, metastatic cancer can shrink significantly or even become undetectable on scans, a state often called remission or having “no evidence of disease” (NED). Maintenance therapy is usually continued to try to prolong this state.
How do I talk to my family about my diagnosis?
Be honest about what you know and what is uncertain. Share your feelings and tell them how they can help, whether it’s with practical tasks or just listening. Consider having your doctor or a social worker present for a family meeting to explain medical details.
The landscape of metastatic cancer is one of both profound challenge and remarkable hope. Medical science has transformed it from an acute, rapidly declining condition to a more manageable chronic disease for many. Success hinges on precise diagnosis, personalized treatment, robust supportive care, and a holistic approach to living. By actively partnering with a dedicated healthcare team, utilizing available resources, and focusing on quality of life, individuals can navigate this complex journey with resilience and purpose.