What Happens If You Don’t Sign Up for Medicare at 65
Turning 65 is a major milestone, and for most Americans, it triggers your Initial Enrollment Period for Medicare. This seven-month window is your first and often best chance to enroll without penalty. But what if you’re still working, covered by a spouse’s plan, or simply unsure? The decision to delay Medicare enrollment is not one to take lightly. While it can be the right choice in specific circumstances, failing to understand the rules can lead to lifelong financial penalties, gaps in coverage, and significant stress. This guide will walk you through the critical consequences of not signing up for Medicare at 65, the exceptions that protect you, and the steps you must take to safeguard your health and finances.
Understanding the Medicare Initial Enrollment Period
Your Medicare Initial Enrollment Period (IEP) is a seven-month window that begins three months before the month you turn 65, includes your birthday month, and ends three months after. This is the foundational rule for Medicare enrollment. During this period, you can sign up for Medicare Part A (hospital insurance), Part B (medical insurance), and Part D (prescription drug coverage) without answering medical questions and, crucially, without facing late enrollment penalties. The system is designed to be straightforward if you enroll on time. However, life is rarely straightforward. Many people assume they can enroll anytime after 65 without issue, but that is a dangerous misconception. The rules for delaying are strict and hinge on having what Medicare considers “creditable coverage” from another source.
The Consequences of Late Enrollment in Medicare Part B
If you do not have creditable coverage and you fail to sign up for Medicare Part B during your IEP, you will face two significant consequences: a lifelong late enrollment penalty and a gap in coverage. The Part B penalty is calculated as 10% of the standard Part B premium for each full 12-month period you were eligible but didn’t enroll. This penalty lasts for as long as you have Medicare Part B. For example, if you delay enrollment for two years without creditable coverage, you will pay a 20% penalty on top of your monthly Part B premium. Given that premiums rise annually, this penalty becomes a substantial and permanent addition to your healthcare costs.
Furthermore, you can only enroll in Part B during the General Enrollment Period (January 1 to March 31 each year), with coverage not starting until July 1. This creates a potential coverage gap of several months where you are liable for all your medical bills. The financial risk of this gap, combined with the permanent penalty, makes delaying Part B without qualifying coverage one of the costliest mistakes a retiree can make.
The High Cost of Delaying Medicare Part D
Similar to Part B, Medicare Part D (prescription drug coverage) carries a late enrollment penalty if you go 63 consecutive days or more without creditable drug coverage after your IEP ends. Creditable drug coverage is typically offered by an employer or union plan that is as good as or better than standard Part D coverage. The Part D penalty is calculated by multiplying 1% of the “national base beneficiary premium” ($34.70 in 2024) by the number of full, uncovered months you were eligible. This amount is then added to your monthly Part D premium for as long as you have coverage.
For instance, if you were without creditable coverage for 24 months, your penalty would be 24% of $34.70, or about $8.33 per month, added to whatever plan premium you choose. This penalty may seem small, but it is also permanent and adjusts with the national base premium. The rules here are particularly tricky because even if you have health insurance that covers medical services, it may not qualify as creditable for prescription drugs. You must get a written notice from your plan administrator confirming your drug coverage is creditable.
When Is It Okay to Delay Medicare Enrollment?
You can safely delay enrolling in Medicare Parts B and D without penalty if you have creditable health coverage from another source. The most common scenarios involve employer-sponsored health insurance. However, the rules differ based on the size of your employer.
If you or your spouse are actively working for a company with 20 or more employees, the employer’s group health plan is primary, and Medicare is secondary. You can delay Part B and Part D without penalty as long as you remain covered. You will have a Special Enrollment Period (SEP) to sign up for Medicare when that employment or coverage ends. This SEP lasts for eight months and allows you to avoid the late penalties.
If the employer has fewer than 20 employees, Medicare typically becomes primary at age 65. In this case, you likely need to enroll in Part A and Part B during your IEP to avoid penalties and coverage denials, as your small employer plan may require it. You must confirm the specific rules with your employer’s benefits administrator.
Other types of creditable coverage can include TRICARE for military retirees or coverage from the Veterans Affairs (VA) system. However, VA benefits do not count as creditable coverage for Part D, creating a potential pitfall for veterans who rely solely on the VA for prescriptions.
Key Steps to Take If You Plan to Delay
If you believe you qualify to delay Medicare, you must take proactive steps to verify your situation and document it. Do not rely on assumptions. First, contact your employer’s benefits administrator to get a written letter stating that your health and drug coverage is creditable under Medicare rules. Second, understand the timeline for your Special Enrollment Period, which is triggered when your employment ends or your coverage ceases, whichever happens first. Mark this date on your calendar. Finally, even if delaying Part B, many people choose to enroll in Medicare Part A at 65 because it is usually premium-free and can provide secondary coverage to your employer plan, potentially lowering out-of-pocket costs.
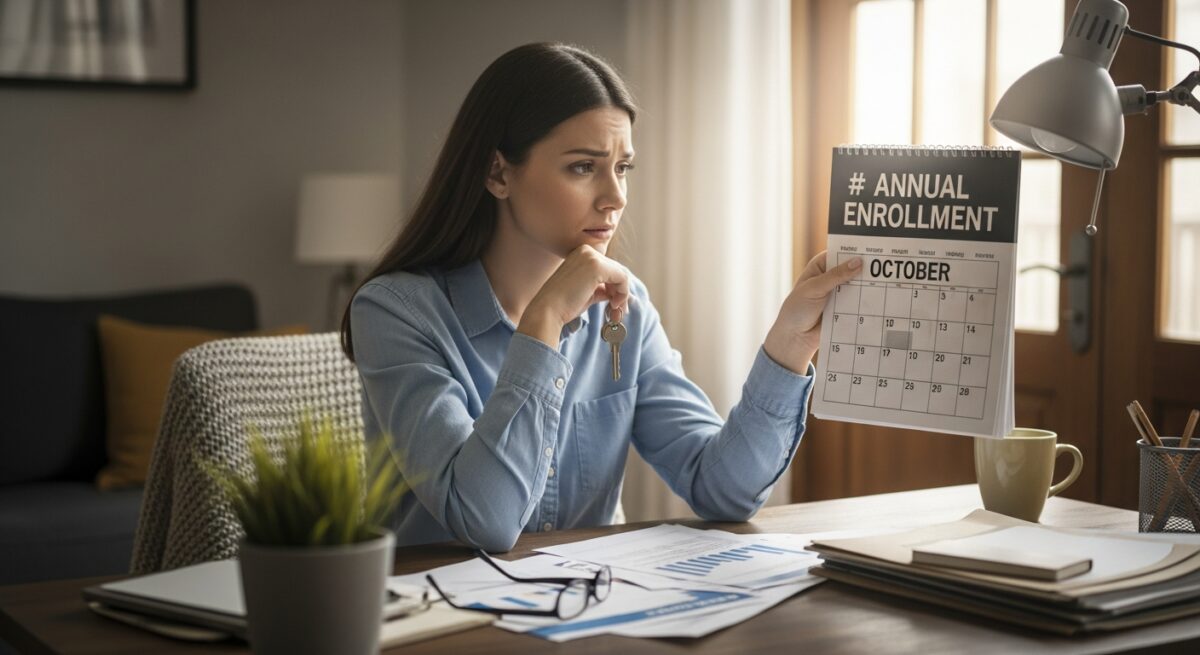
Navigating the Special Enrollment Period
The Special Enrollment Period (SEP) is your safety net if you delay Medicare with creditable coverage. It is an eight-month window that begins the month after your employment ends or your group health coverage ends, whichever happens first. It is critical not to miss this window. During the SEP, you can enroll in Medicare Part B and Part D without penalty. Your coverage will begin the first day of the month after you apply. For example, if your coverage ends on June 30 and you apply in July, your Medicare will start August 1.
A common and costly error is confusing the SEP with the General Enrollment Period. If you miss your SEP, you must wait for the next General Enrollment Period (January-March), face lifelong late penalties, and experience a coverage gap. Therefore, planning the transition from employer coverage to Medicare is essential. Consider applying for Medicare a month or two before your employer coverage ends to ensure a seamless transition with no gap in protection.
Frequently Asked Questions
What happens if I only delay Part B but take Part A at 65?
This is a common and often recommended strategy if you have creditable coverage. Since Part A is usually premium-free, enrolling in it can provide secondary hospital coverage. Delaying Part B allows you to avoid its monthly premium while you’re still covered by an employer plan. Just be sure to enroll in Part B during your Special Enrollment Period when your other coverage ends.
I have retiree health benefits from my former employer. Can I delay Medicare?
No. Retiree coverage is not considered creditable coverage for the purpose of avoiding late enrollment penalties. You must enroll in Medicare Parts A and B during your Initial Enrollment Period at 65. Your retiree plan will then act as a supplement to Medicare, often covering copays and deductibles.
Does COBRA count as creditable coverage?
No. COBRA and the health insurance marketplace (Affordable Care Act plans) are not considered creditable coverage for Medicare Part B. If you enroll in COBRA after age 65, you will not qualify for a Special Enrollment Period when that COBRA ends. You will face late penalties and be forced to wait for the General Enrollment Period.
How do I prove I had creditable coverage to avoid penalties?
If you enroll late, Medicare will send you a penalty notice. You must then submit Form CMS-1763 (Request for Employment Information) to Social Security, which your employer must complete. This form proves you had qualifying coverage. It is far easier to get the written notice from your employer before you delay.
Can I be denied Medicare coverage if I enroll late?
No. Medicare does not underwrite or deny coverage based on health status. You are guaranteed issuance during any enrollment period. However, you will be subject to the financial penalties discussed, and you may have a waiting period before coverage starts.
The decision to enroll in Medicare at 65 is a pivotal one with long-term implications. While delaying can be appropriate under the shield of active, creditable employer coverage, navigating the rules requires diligence and verification. The risks of getting it wrong, namely permanent monthly penalties and dangerous gaps in health insurance, are too significant to ignore. By understanding the difference between your Initial Enrollment Period, Special Enrollment Period, and General Enrollment Period, and by securing proof of your coverage status, you can make an informed choice that protects both your health and your financial future. For personalized guidance, always consult with the Social Security Administration or a licensed Medicare advisor.