Understanding Rectal Cancer Symptoms, Diagnosis, and Treatment
A persistent change in bowel habits, a feeling of incomplete evacuation, or blood in the stool: these subtle signs can be the first indicators of a significant health concern, rectal cancer. While sharing many similarities with colon cancer and often grouped together as colorectal cancer, rectal cancer presents unique challenges due to its location in the last several inches of the large intestine, the rectum. This area’s confined space within the pelvis, surrounded by other critical structures, influences everything from symptoms to complex treatment strategies. Early detection is profoundly impactful, transforming a potentially life-threatening diagnosis into a highly treatable condition. This guide provides a detailed overview of rectal cancer, from its initial warning signs to the latest advances in multimodal therapy, empowering you with knowledge for informed health decisions.
What Is Rectal Cancer and How Does It Develop?
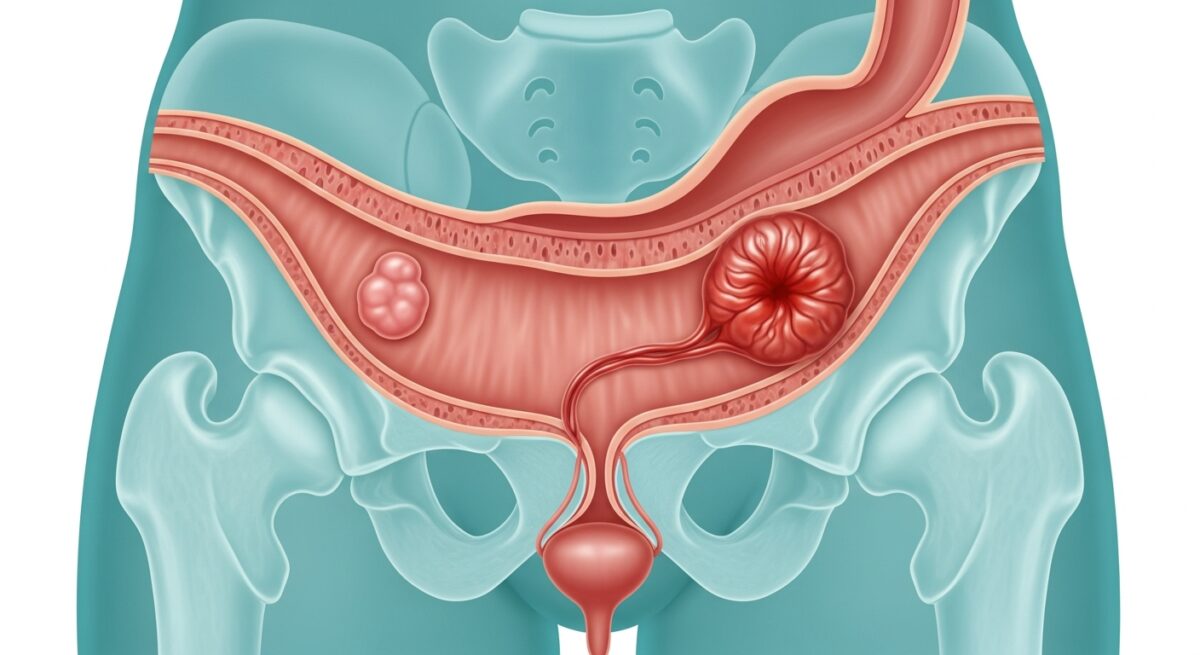
Rectal cancer begins when healthy cells in the lining of the rectum develop errors in their DNA. These errors cause cells to grow uncontrollably and continue living when normal cells would die. This accumulating mass of abnormal cells can form a tumor and, over time, invade nearby healthy tissue and spread to other parts of the body. Most rectal cancers start as benign polyps, specifically adenomatous polyps. Not all polyps become cancerous, but the adenomatous type is considered pre-cancerous. The progression from a polyp to cancer can take many years, which creates a critical window for detection and removal during screening procedures like a colonoscopy.
The rectum’s primary function is to store stool until it is ready to be expelled. Its anatomical position, low in the pelvis and adjacent to other organs like the prostate in men and the vagina in women, makes surgical and radiation treatment more intricate than for cancers higher in the colon. Understanding this distinction is key for patients and families navigating a diagnosis, as treatment protocols are specifically tailored for rectal tumors.
Recognizing the Signs and Symptoms
Symptoms of rectal cancer can be easy to dismiss or attribute to more common conditions like hemorrhoids or irritable bowel syndrome. However, persistence and combination of symptoms warrant prompt medical evaluation. A hallmark sign is a persistent change in bowel habits, which may include diarrhea, constipation, or a change in the consistency of stool. This change typically lasts for more than a few days. Another common symptom is rectal bleeding, which may appear as bright red blood on toilet paper or in the toilet bowl. It is crucial not to assume rectal bleeding is solely from hemorrhoids without a professional assessment.
Patients often report a persistent feeling of needing to have a bowel movement that is not relieved by doing so, known as tenesmus. Other symptoms can include abdominal discomfort, such as cramps, gas, or pain. Unexplained weight loss, weakness, fatigue, and a feeling that the bowel does not empty completely are also potential indicators. In more advanced stages, symptoms may include pelvic pain or pain during bowel movements. Because these signs are non-specific, consulting a healthcare provider for a proper evaluation is the essential first step. For a deeper exploration of navigating health coverage for such diagnostic tests, you can Read full article on related insurance topics.
Key Risk Factors and Prevention Strategies
While the exact cause of rectal cancer is not always clear, several well-established risk factors increase an individual’s likelihood of developing the disease. Some factors are non-modifiable, such as increasing age (most cases are diagnosed after 50), a personal history of colorectal polyps or cancer, a family history of colorectal cancer, and inherited syndromes like Lynch syndrome or familial adenomatous polyposis (FAP). Inflammatory bowel diseases, such as Crohn’s disease or ulcerative colitis affecting the rectum, also elevate risk.
Importantly, many risk factors are related to lifestyle and are modifiable. A diet high in red and processed meats and low in fruits, vegetables, and whole grains is associated with higher risk. Physical inactivity, obesity, smoking, and heavy alcohol use are also significant contributors. Therefore, prevention strategies focus heavily on lifestyle modifications. Adopting a diet rich in fiber, vitamins, and antioxidants, maintaining a healthy weight through regular exercise, avoiding tobacco, and limiting alcohol consumption are powerful proactive steps. Furthermore, for individuals at average risk, regular screening beginning at age 45 is the most effective preventive measure, as it allows for the identification and removal of polyps before they become cancerous.
The Diagnostic Process for Rectal Cancer
When symptoms or screening tests suggest the possibility of rectal cancer, a systematic diagnostic process is initiated to confirm the presence of cancer and determine its extent, or stage. The cornerstone of diagnosis is a colonoscopy. During this procedure, a long, flexible tube with a camera is used to examine the entire colon and rectum. If any suspicious areas are found, the doctor can take tissue samples, or biopsies, for laboratory analysis. A pathology report confirming cancer cells is necessary for a definitive diagnosis.
Once cancer is confirmed, staging tests are crucial. These may include:
- Imaging Tests: A CT scan of the chest, abdomen, and pelvis checks for spread to distant organs like the liver or lungs. A pelvic MRI provides a highly detailed image of the rectal tumor and its relationship to surrounding structures, which is vital for planning surgery and radiation.
- Endorectal Ultrasound: This test uses a special probe inserted into the rectum to assess how deeply the tumor has invaded the rectal wall and whether nearby lymph nodes are involved.
- Blood Tests: While no blood test diagnoses rectal cancer, tests for carcinoembryonic antigen (CEA) can be useful. Elevated CEA levels may indicate cancer and can be used to monitor response to treatment.
Staging follows the TNM system (Tumor, Node, Metastasis), which classifies the depth of tumor invasion, lymph node involvement, and presence of distant metastasis. Accurate staging, from Stage 0 (cancer in situ) to Stage IV (metastatic cancer), directly guides the treatment plan.
Modern Treatment Approaches and Advances
Treatment for rectal cancer is highly personalized and typically involves a multidisciplinary team of surgeons, medical oncologists, and radiation oncologists. The approach depends primarily on the stage and location of the tumor. For very early-stage cancers confined to a polyp, removal during a colonoscopy may be sufficient. For most other non-metastatic cancers, a combination of therapies, known as multimodal therapy, is standard.
For locally advanced rectal cancer (Stages II and III), the current standard of care in many cases is neoadjuvant therapy, meaning treatment given before surgery. This often involves a combination of chemotherapy and radiation therapy, called chemoradiation, administered over several weeks. This approach aims to shrink the tumor, making it easier to remove completely, and to reduce the risk of local recurrence. Following this, surgery is performed. The type of surgery can range from a local excision for small tumors to a more extensive procedure like a low anterior resection (LAR) or an abdominoperineal resection (APR), which may require a permanent or temporary colostomy. After surgery, adjuvant chemotherapy is usually recommended to eliminate any remaining microscopic cancer cells.
Advances in surgical techniques, such as minimally invasive laparoscopic and robotic surgery, have led to faster recovery times and reduced complications. For metastatic (Stage IV) rectal cancer, treatment focuses on systemic therapies like chemotherapy, targeted therapy, and immunotherapy to control the disease and prolong life, sometimes in combination with surgery or radiation for specific sites of metastasis.
Frequently Asked Questions
What is the difference between colon cancer and rectal cancer?
While they are collectively called colorectal cancer and share many risk factors, they are distinguished by location. Colon cancer occurs in the large intestine (colon), while rectal cancer is in the last several inches leading to the anus. This anatomical difference affects symptoms, surgical complexity, and sometimes treatment protocols, particularly the use of radiation therapy, which is more common for rectal tumors.
At what age should I start screening for rectal cancer?
For people at average risk, major guidelines recommend starting regular screening at age 45. If you have a family history or other risk factors (like inflammatory bowel disease), you may need to start earlier and be screened more frequently. Discuss your personal risk profile with your doctor.
Can rectal cancer be cured?
Yes, especially when detected early. The five-year survival rate for localized rectal cancer (confined to the rectum) is high. Even for regional cancers that have spread to nearby lymph nodes, modern multimodal treatment offers a strong chance for cure. Early detection through screening is the most powerful tool for a cure.
What are the side effects of common treatments?
Side effects vary by treatment. Surgery may lead to temporary or permanent changes in bowel function or require an ostomy. Radiation can cause fatigue, skin irritation, and bowel or bladder issues. Chemotherapy side effects often include nausea, fatigue, and lowered blood counts. Your care team will provide detailed management plans for these effects.
Is a colostomy always necessary for rectal cancer surgery?
No. Many patients undergo surgery that reconnects the bowel, allowing for normal passage of stool. A permanent colostomy is more likely if the tumor is very low in the rectum, near the anal sphincter. Often, a temporary colostomy is created to allow the surgical connection to heal, which is reversed in a subsequent operation.
Facing a rectal cancer diagnosis is a profound challenge, but it is one met with increasingly sophisticated and effective medical strategies. From enhanced screening guidelines that catch pre-cancerous growths to precision surgical techniques and tailored chemoradiation, the outlook for patients continues to improve. The journey underscores the irreplaceable value of proactive health management: knowing your risk factors, adhering to recommended screenings, and seeking prompt medical attention for concerning symptoms. With a dedicated medical team and a comprehensive treatment plan, many individuals navigate this diagnosis successfully and return to a full, active life.