Understanding Neuroendocrine Cancer: Symptoms, Types, and Treatments
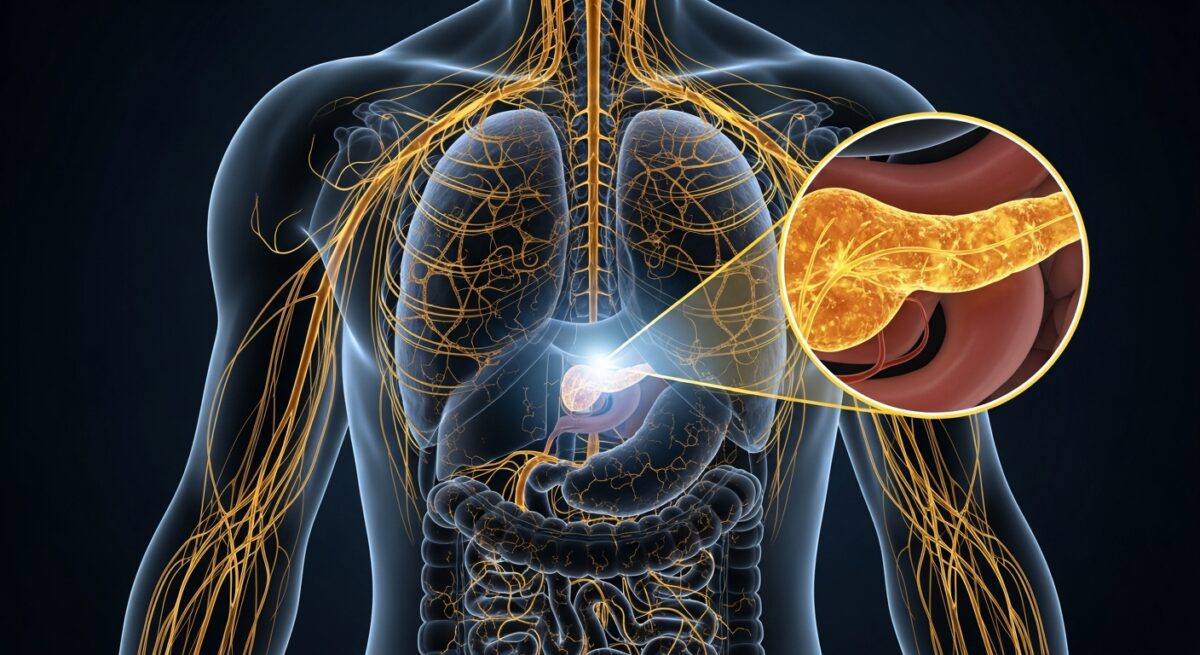
Neuroendocrine cancer, also known as neuroendocrine tumors (NETs), represents a complex and often misunderstood group of malignancies that arise from cells which release hormones into the bloodstream in response to signals from the nervous system. These rare tumors can occur anywhere in the body but are most commonly found in the gastrointestinal tract, lungs, and pancreas. Due to their ability to produce hormones, NETs can cause a wide array of unusual symptoms that often lead to misdiagnosis, sometimes for years. This article provides a comprehensive look at neuroendocrine cancer, aiming to demystify its diagnosis, treatment pathways, and the unique challenges it presents. Understanding this disease is the first step toward effective management and improved patient outcomes.
What Is Neuroendocrine Cancer?
Neuroendocrine tumors originate from specialized cells called neuroendocrine cells. These cells share characteristics with both nerve cells (neurons) and hormone-producing (endocrine) cells. They are found throughout the body, particularly in organs like the intestines, lungs, and pancreas, where they help control the release of digestive juices, air flow, and blood flow. When these cells develop genetic mutations and begin to divide uncontrollably, they form neuroendocrine tumors. NETs are classified by their grade and stage, which heavily influence prognosis and treatment. Grade refers to how quickly the cells are dividing (from low-grade, slow-growing, to high-grade, aggressive). Stage describes the size of the tumor and how far it has spread, a critical factor in determining the treatment approach.
These cancers are notably heterogeneous. Some are functional, meaning they secrete hormones like serotonin, insulin, or gastrin, leading to distinct clinical syndromes. Others are non-functional and may not cause symptoms until they grow large or spread. The diversity of NETs necessitates a highly personalized approach to care, involving a multidisciplinary team of oncologists, endocrinologists, surgeons, and radiologists. Diagnosis often involves a combination of blood tests, imaging scans (such as CT, MRI, or specialized DOTATATE PET scans), and biopsy.
Common Symptoms and Diagnostic Challenges
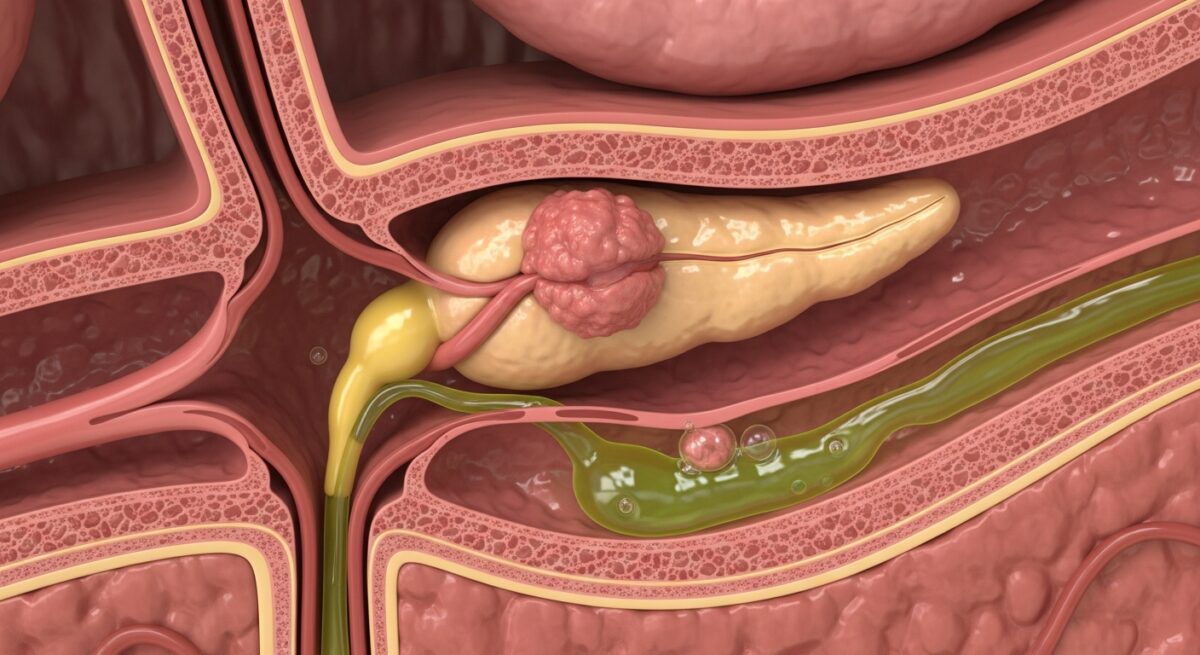
The symptoms of neuroendocrine cancer are notoriously vague and can mimic many more common conditions, which is why these tumors are frequently called “great masqueraders.” For functional tumors, symptoms are directly related to the type of hormone being overproduced. Carcinoid syndrome, associated with tumors in the digestive tract that have spread to the liver, can cause flushing of the skin, diarrhea, wheezing, and heart valve problems. A pancreatic NET that secretes insulin might cause severe hypoglycemia (low blood sugar), leading to confusion, sweating, and dizziness.
Non-functional tumors may not cause any symptoms in their early stages. As they grow, they can lead to pain, a palpable mass, fatigue, or unintended weight loss. Because symptoms like diarrhea, flushing, or abdominal pain are common to many ailments (like irritable bowel syndrome or menopause), patients often face a long and frustrating diagnostic journey. The average time from symptom onset to a correct NET diagnosis can be several years. This delay underscores the importance of physician awareness and the need for patients with persistent, unexplained symptoms to seek evaluation from specialists.
Primary Treatment Options and Management Strategies
Treatment for neuroendocrine cancer is highly individualized and depends on the tumor’s location, grade, stage, whether it is functional, and the patient’s overall health. There is no one-size-fits-all approach. The management strategy often involves a combination of modalities aimed at controlling tumor growth, managing hormone-related symptoms, and preserving quality of life.
Surgery is the only potentially curative treatment and is the preferred option for localized neuroendocrine tumors. The goal is to completely remove the primary tumor and any affected lymph nodes. For advanced or metastatic disease, surgery may still be used to debulk the tumor (remove as much as possible) to alleviate symptoms or prevent complications. When surgery is not an option, other systemic and localized treatments come into play. These include somatostatin analog injections (like octreotide or lanreotide), which can control hormone-related symptoms and slow tumor growth. For more information on navigating complex treatment decisions and associated healthcare coverage, Read full article provides additional details.
Other key treatment options include:
- Targeted Therapy: Drugs like everolimus and sunitinib interfere with specific pathways that tumor cells use to grow and survive.
- Peptide Receptor Radionuclide Therapy (PRRT): A specialized radiation treatment that delivers a radioactive molecule directly to NET cells, often used for tumors expressing somatostatin receptors.
- Chemotherapy: Generally reserved for high-grade, aggressive neuroendocrine carcinomas.
- Liver-Directed Therapies: For tumors that have spread to the liver, options like embolization, radioembolization, or ablation can help control disease in that organ.
Ongoing monitoring through scans and biomarker tests is a cornerstone of long-term management, as NETs can be chronic conditions requiring years of surveillance and treatment adjustments.
Frequently Asked Questions About Neuroendocrine Cancer
Is neuroendocrine cancer always malignant?
Not all neuroendocrine tumors are cancerous. Some are benign and grow slowly without spreading. However, even low-grade malignant NETs have the potential to metastasize over time, which is why expert evaluation and monitoring are essential.
What is the life expectancy for someone with a neuroendocrine tumor?
Prognosis varies dramatically based on the tumor’s grade, stage, location, and how well it responds to treatment. Many patients with low-grade, localized NETs have a normal or near-normal life expectancy. Even with advanced disease, newer treatments have significantly improved survival and quality of life, allowing many to manage their condition as a chronic illness for years.
Are neuroendocrine tumors hereditary?
Most NETs are sporadic, meaning they occur by chance. However, a minority (about 10%) are associated with inherited genetic syndromes, such as Multiple Endocrine Neoplasia type 1 (MEN1), von Hippel-Lindau syndrome (VHL), or Neurofibromatosis type 1 (NF1). Genetic counseling may be recommended if there is a strong family history.
Can diet affect neuroendocrine cancer?
While no specific diet cures NETs, dietary management can be crucial for controlling symptoms, especially for functional tumors. For example, avoiding large meals, alcohol, and spicy foods may help reduce carcinoid syndrome flushing. Patients with specific hormone-related issues should work with a dietitian familiar with NETs.
Navigating a neuroendocrine cancer diagnosis involves understanding a rare and complex disease landscape. With advances in diagnostic imaging, targeted therapies, and a growing network of specialists, patient outlooks continue to improve. The key lies in obtaining an accurate diagnosis, seeking care from a team experienced with NETs, and actively participating in a tailored, long-term management plan. Continued research offers hope for even more effective treatments on the horizon.