Recognizing Bladder Cancer Symptoms: Key Signs and Next Steps
Noticing a change in your body, especially when it involves something as fundamental as urination, can be unsettling. While many urinary symptoms are caused by common, non-cancerous conditions like infections or an enlarged prostate, they can also be the first warning signs of bladder cancer. Understanding these symptoms is crucial, as early detection significantly improves treatment outcomes and survival rates. This guide provides a detailed look at the potential symptoms of bladder cancer, explains what they mean, and outlines the logical steps to take if you experience them.
The Primary Warning Sign: Hematuria
The most common and often the first symptom of bladder cancer is hematuria, or blood in the urine. This sign is present in the vast majority of diagnosed cases. It is important to understand that hematuria can manifest in two distinct ways, each carrying its own level of urgency. Gross hematuria refers to blood that is visible to the naked eye. The urine may appear pink, red, or cola-colored. Sometimes, passing visible blood can be startling, but it may also come and go, leading some to dismiss it after it clears. Microscopic hematuria, on the other hand, is only detectable under a microscope during a urinalysis. The urine looks normal, but the test reveals the presence of red blood cells. This form is often discovered incidentally during a routine check-up for another issue. Regardless of visibility, any presence of blood in the urine warrants a prompt medical evaluation to determine the cause. It is never a symptom to ignore.
Changes in Urinary Habits and Sensations
Beyond visible blood, bladder cancer can irritate the bladder wall, leading to a cluster of symptoms that mimic a urinary tract infection (UTI). These changes are often more subtle but persistent. A key differentiator is that these symptoms do not resolve with standard antibiotic treatment if cancer is the underlying cause. The most frequent changes in urinary habits include a sudden, urgent need to urinate, even when the bladder is not full. You may also experience increased frequency, needing to urinate many more times during the day and night than usual. Dysuria, or a burning or painful sensation during urination, is another common complaint. Some individuals may also feel a persistent need to urinate without being able to pass much, or they may experience a weak urine stream or difficulty starting urination. While our guide on bladder cancer symptoms and critical signs delves deeper into these irritative changes, the persistent nature of these issues is what should prompt further investigation.
Advanced and Non-Urinary Symptoms
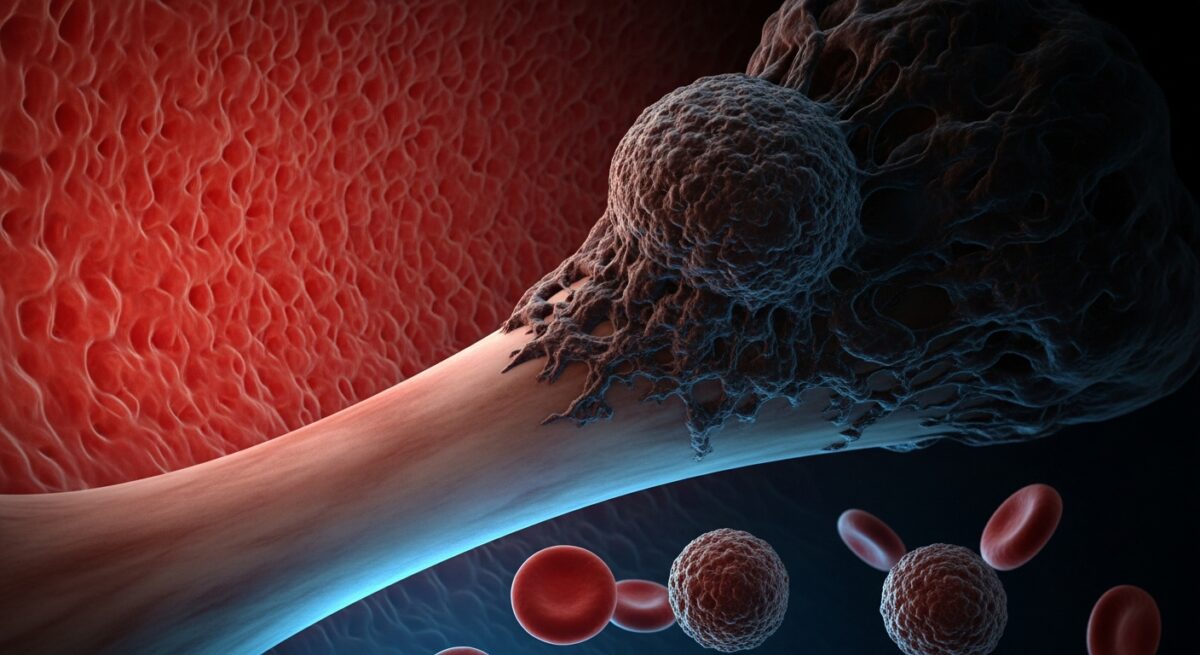
When bladder cancer grows larger or begins to spread beyond the lining of the bladder, it can cause a different set of symptoms. These are often signs of more advanced disease and underscore why early detection based on initial urinary symptoms is so vital. Advanced symptoms can include persistent pain in one side of the lower back, which may indicate that the cancer is affecting the kidneys or ureters. Pelvic pain can also develop. A significant and unintentional loss of appetite and weight is a systemic symptom that can occur with many advanced cancers, including bladder cancer. You may feel constantly fatigued or weak, a tiredness that is not relieved by rest. Swelling in the feet can occur if the cancer disrupts normal lymphatic drainage. Bone pain may be a sign that the cancer has metastasized to the bones. The appearance of these symptoms typically means the cancer is no longer in its earliest, most treatable stages, making the recognition of initial signs even more critical.
Risk Factors and When to See a Doctor
Knowing the symptoms is one part of the equation, understanding your personal risk is another. Certain factors significantly increase the likelihood of developing bladder cancer. Smoking is the single greatest risk factor, responsible for about half of all cases. The chemicals in tobacco smoke are absorbed into the bloodstream, filtered by the kidneys, and concentrated in the urine, where they can damage the bladder lining over time. Occupational exposure to certain chemicals used in dye, rubber, leather, paint, and printing industries is another major risk. Other factors include chronic bladder inflammation (such as from long-term catheter use), a personal or family history of bladder cancer, previous cancer treatments involving radiation to the pelvis or certain chemotherapy drugs, and being male and older, as most cases are diagnosed in people over 55.
Given these risks and symptoms, it is essential to know when to seek professional medical advice. You should consult a doctor if you experience any of the following:
- Visible blood in your urine (red, pink, or cola-colored)
- Urinary symptoms (pain, frequency, urgency) that persist despite treatment for a suspected infection
- Persistent lower back or pelvic pain without another clear cause
- Any other concerning change in your urinary patterns or overall health
Do not wait for symptoms to worsen or for new ones to appear. Early consultation can lead to earlier diagnosis and a wider range of effective treatment options. A healthcare provider will likely start with a detailed medical history, a physical exam, and a urinalysis. If indicated, further diagnostic steps like a cystoscopy (using a thin scope to look inside the bladder) or imaging tests may be recommended.
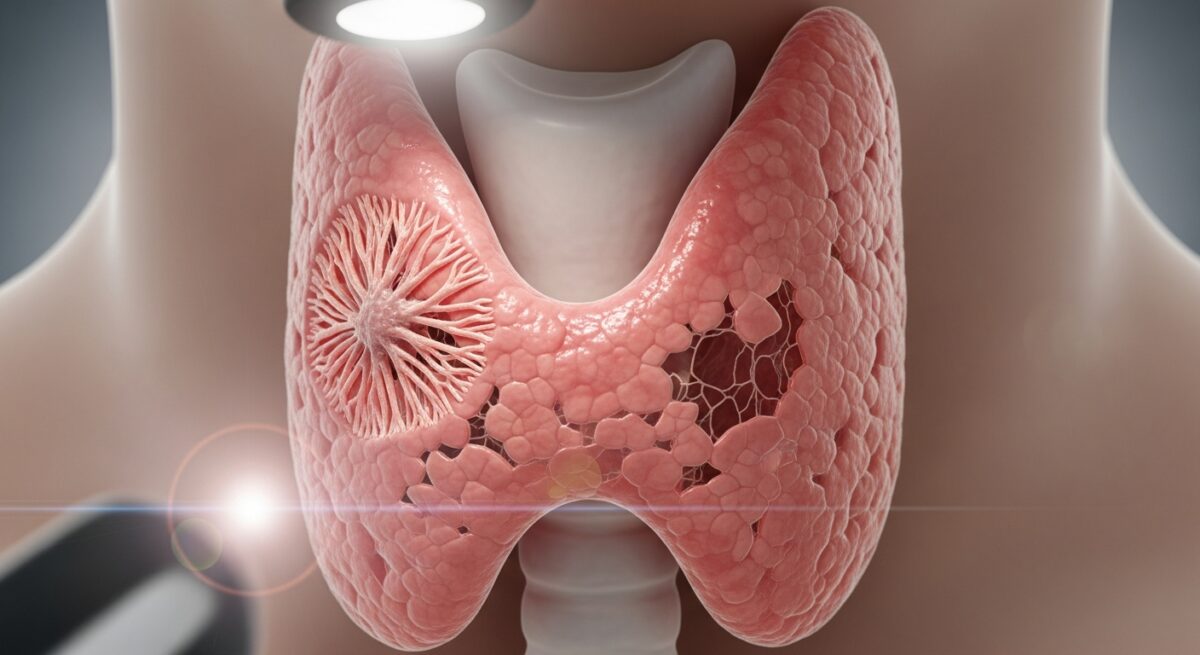
Diagnosis, Treatment, and the Role of Medicare
The diagnostic journey typically begins with non-invasive tests. A urinalysis can confirm the presence of blood and check for infection. A urine cytology exam looks for cancer cells shed into the urine. If these raise suspicion, a cystoscopy is the gold standard procedure. During this, a urologist inserts a cystoscope through the urethra to view the bladder lining. If any abnormal areas are seen, a biopsy can be taken. Imaging tests like CT scans or ultrasounds help determine if the cancer has spread beyond the bladder.
Treatment depends heavily on the stage and grade of the cancer. For early-stage, non-invasive cancers, treatment often involves a procedure called transurethral resection of bladder tumor (TURBT) to remove the tumor, sometimes followed by intravesical therapy (medication placed directly into the bladder) to kill any remaining cancer cells. For more advanced cancers that have invaded the muscle layer of the bladder, treatment may include radical cystectomy (surgical removal of the bladder), chemotherapy, radiation therapy, or immunotherapy. Newer targeted therapies and immunotherapies have significantly improved outcomes for many patients.
Navigating cancer diagnosis and treatment is challenging, and understanding your health coverage is a practical necessity. Medicare provides essential benefits that cover many aspects of cancer care, from diagnostic tests and doctor visits to hospital stays, surgeries, and approved chemotherapy drugs. Understanding the specifics of your plan, whether Original Medicare or a Medicare Advantage plan, is key to managing costs. For a comprehensive look at how different plans can support you through a cancer journey, including coverage for specialists and treatments, exploring resources on the best Medicare Advantage plans for comprehensive care can be highly informative.
Frequently Asked Questions
Can you have bladder cancer with no symptoms? In its very early stages, bladder cancer, particularly microscopic hematuria, may cause no noticeable symptoms. This is why routine check-ups that include a urinalysis can be valuable, especially for individuals with known risk factors.
Is blood in the urine always cancer? No, it is not. Many conditions can cause hematuria, including urinary tract infections, kidney stones, an enlarged prostate, or vigorous exercise. However, because it is the leading symptom of bladder cancer, it must always be evaluated by a doctor to rule out serious causes.
What does bladder cancer pain feel like? In early stages, there is often no pain. When pain does occur, it may feel like a persistent burning during urination. In advanced stages, pain may be felt as a deep ache in the lower back, sides, or pelvis.
How quickly do bladder cancer symptoms progress? The progression varies widely. Some low-grade cancers grow very slowly and may cause intermittent symptoms over a long period. High-grade cancers can be more aggressive, with symptoms becoming more persistent and pronounced more quickly. Never gauge urgency based on perceived speed, any symptom warrants prompt attention.
Can lifestyle changes reduce my risk? Absolutely. The most impactful step is to not smoke or to quit smoking. Minimizing exposure to occupational chemicals with proper protective equipment, drinking plenty of fluids (especially water) throughout the day, and eating a diet rich in fruits and vegetables may also contribute to lower risk.
Recognizing the symptoms of bladder cancer is a powerful form of self-advocacy. While the signs can be subtle or mistaken for less serious conditions, listening to your body and acting on persistent changes is essential. Hematuria, changes in urinary habits, and later-stage symptoms like back pain are all signals that require professional medical evaluation. With early detection, bladder cancer is highly treatable. Do not hesitate to become your own health advocate, discuss any concerns openly with your doctor, and ensure you undergo the recommended tests to achieve clarity and peace of mind. Your proactive approach can make a definitive difference in your health journey.