Pancreatic Cancer Symptoms: What to Watch For
Pancreatic cancer is often called a silent disease because its symptoms are typically vague, easily mistaken for more common conditions, and frequently appear only in later stages. This delay in recognition is a primary reason why pancreatic cancer has one of the lowest survival rates among major cancers. However, being informed about the potential signs, understanding their nuances, and knowing when to seek medical evaluation can be life-saving. This knowledge empowers individuals and their families to advocate for timely investigation, which is critical for improving outcomes.
Understanding the Pancreas and Why Symptoms Are Subtle
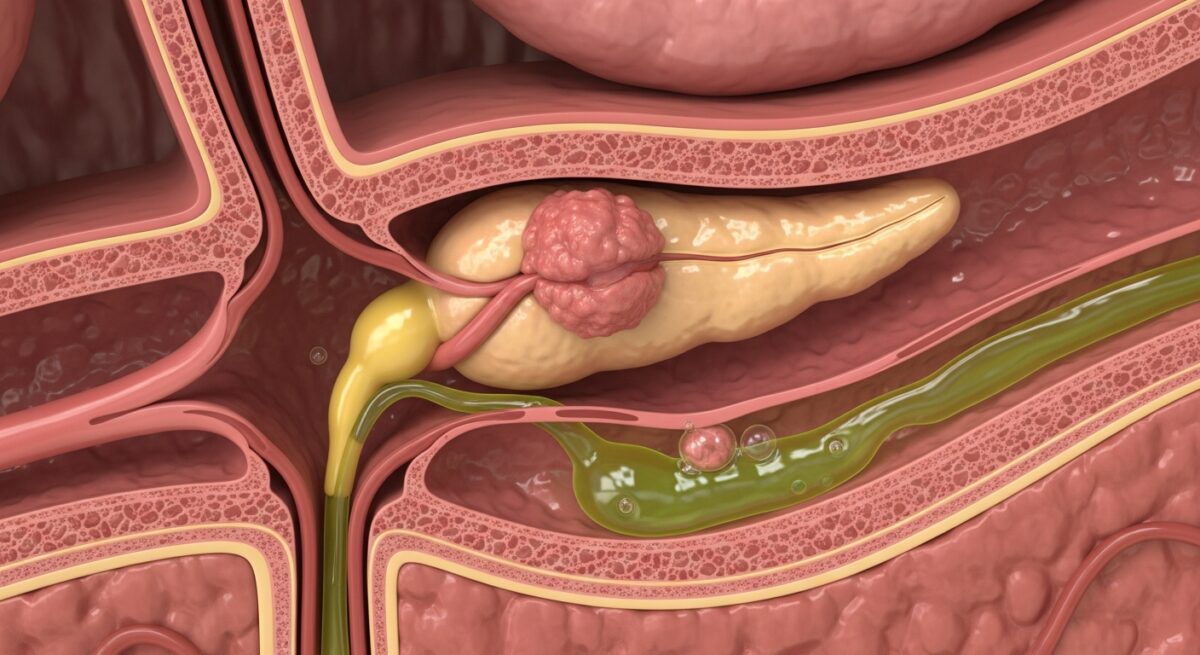
The pancreas is a six-inch-long organ located deep in the abdomen, behind the stomach and in front of the spine. It plays a dual role: it produces digestive enzymes (exocrine function) and hormones like insulin (endocrine function). Its deep, central location means a tumor can grow for some time without pressing on nerves or organs that would cause noticeable pain. Furthermore, the pancreas has a significant functional reserve, meaning it can continue working adequately even when a portion is compromised by a tumor. This biological reality is why pancreatic cancer symptoms are often non-specific and develop insidiously. Many early signs are related to the tumor blocking the bile duct or pancreatic duct, or affecting the stomach, rather than from the cancer itself causing direct pain initially.
The Most Common Symptoms of Pancreatic Cancer
The presentation of pancreatic cancer varies depending on the tumor’s location within the organ (head, body, or tail). Tumors in the head of the pancreas, which are more common, tend to cause symptoms earlier because they can block the common bile duct. Symptoms from tumors in the body or tail often appear later, making them particularly dangerous. The most frequent symptoms collectively form a pattern that, while not diagnostic on its own, should prompt further medical investigation, especially if they are new, persistent, and worsening.
Jaundice: A Key Warning Sign
Jaundice is the yellowing of the skin and the whites of the eyes. It is often one of the first noticeable symptoms, particularly for tumors in the head of the pancreas. This occurs when the tumor blocks the bile duct, causing a buildup of bilirubin, a substance produced by the liver. Jaundice is usually painless but is accompanied by other telltale changes. The urine often becomes dark, like the color of tea or cola, because the excess bilirubin is excreted by the kidneys. Stools may become pale, clay-colored, or greasy because bilirubin is not reaching the intestines to give stool its normal brown color. Itching of the skin, medically known as pruritus, is another common companion of jaundice, caused by bile salt deposits in the skin. While jaundice is most commonly associated with liver conditions like hepatitis, its painless onset in an older adult is a major red flag for pancreatic cancer.
Abdominal and Back Pain
Pain is a common but often later symptom. It typically manifests as a dull, nagging ache in the upper abdomen that may radiate to the mid or upper back. This pain occurs as the tumor grows and begins to press on surrounding nerves and organs near the spine. The character of the pain is important: it often worsens when lying down or after eating, and it may be temporarily relieved by leaning forward. This positional nature is a clue that distinguishes it from common back pain. It’s crucial to understand that this type of persistent, deep-seated abdominal or back pain that doesn’t resolve with typical treatments should not be ignored, especially if it’s accompanied by any other symptoms on this list.
Unexplained Weight Loss and Loss of Appetite
Significant, unintentional weight loss is a hallmark of many cancers, including pancreatic cancer. This is not simply losing a few pounds, but a noticeable drop in weight without changes in diet or exercise. Two primary mechanisms drive this. First, cancer cells consume a large amount of the body’s energy resources. Second, and more specific to pancreatic cancer, the tumor can interfere with the pancreas’s ability to produce digestive enzymes. Without these enzymes, the body cannot properly break down and absorb fats and nutrients from food, a condition called exocrine pancreatic insufficiency. This leads to malnutrition and weight loss, even if a person is eating normally. Accompanying this is often a profound loss of appetite or an early feeling of fullness after eating only a small amount, as the tumor can press on the stomach.
Digestive Changes and Associated Symptoms
Beyond weight loss, the disruption of normal pancreatic function leads to several distinct digestive issues. These symptoms are directly tied to the organ’s role in digestion and can serve as important clues.
Nausea and vomiting may occur, particularly if the tumor impedes the normal emptying of the stomach into the small intestine. New-onset diabetes or existing diabetes that becomes suddenly and inexplicably harder to control can be a sign, as the tumor damages insulin-producing cells. Perhaps one of the most characteristic, though less discussed, symptoms is steatorrhea. This is the passage of foul-smelling, oily, or fatty stools that are difficult to flush. They may float or appear greasy. This happens because undigested fat is being excreted. For a deeper exploration of these and other early indicators, our resource on recognizing pancreatic cancer symptoms provides a detailed breakdown.
The following list summarizes key digestive and systemic symptoms that warrant attention:
- New-Onset Diabetes: Especially in individuals over 50 with no family history or risk factors.
- Steatorrhea (Fatty Stools): Pale, oily, foul-smelling stools that float.
- Nausea and Vomiting: Persistent, often related to eating.
- Gallbladder or Liver Enlargement: A blocked bile duct can cause the gallbladder to swell, which a doctor may feel during an exam.
- Blood Clots: Unexplained blood clots in large veins, known as deep vein thrombosis (DVT) or in the lungs (pulmonary embolism), can sometimes be the first sign.
It is the combination of these symptoms that is most telling. For instance, jaundice combined with weight loss and clay-colored stools is far more significant than any one symptom alone.
Less Common but Important Symptoms
While the symptoms above are most frequent, pancreatic cancer can sometimes present in more unusual ways. Being aware of these can help paint a complete clinical picture. Some individuals may experience depression or anxiety that seems to arise without a clear trigger, which some research suggests may be related to the cancer’s biological impact. A rare but notable sign is Trousseau’s sign of malignancy, which is the spontaneous formation of blood clots in unusual places like the arms or neck. Fatigue is almost universal in advanced cancer but can be an early, non-specific complaint. It’s a profound tiredness that isn’t relieved by rest.
Risk Factors and When to See a Doctor
Understanding symptoms must be paired with an awareness of risk factors. These include smoking, chronic pancreatitis, long-standing diabetes, family history of pancreatic cancer or certain genetic syndromes (like BRCA mutations), obesity, and older age (most patients are over 65). Having one or more risk factors does not mean you will get cancer, but it means you should be more vigilant about symptoms.
The critical question is when to seek medical advice. You should consult a healthcare provider if you experience any of the following: jaundice (yellow skin/eyes), persistent abdominal or mid-back pain that doesn’t improve, unexplained weight loss exceeding 5% of your body weight over 6-12 months, new-onset diabetes or loss of blood sugar control, or significant digestive changes like oily stools and loss of appetite. It is essential to be proactive and persistent. Given the vagueness of symptoms, they are often initially attributed to stress, irritable bowel syndrome, or gastritis. If your symptoms persist despite initial management, or if your instinct tells you something is seriously wrong, seek a second opinion or ask for a referral to a gastroenterologist. Clear communication with your doctor is vital; keeping a symptom diary can be incredibly helpful. For Medicare beneficiaries, understanding your coverage for specialist visits and diagnostic tests is crucial for accessing timely care without financial stress. You can explore your options for comprehensive coverage that supports cancer screening and care by choosing to Read full article on planning for health needs.
Diagnostic Process and the Importance of Early Detection
If pancreatic cancer is suspected based on symptoms and physical exam, the diagnostic pathway typically involves imaging and possibly a biopsy. Initial imaging often includes a contrast-enhanced CT scan of the abdomen, which is the most common tool for detecting a pancreatic tumor. An endoscopic ultrasound (EUS), where a small ultrasound probe is passed down into the stomach, provides high-resolution images and allows for a fine-needle biopsy during the same procedure. MRI and specialized MRCP scans can also be used. A blood test for the tumor marker CA 19-9 may be ordered, but it is not reliable for screening as it can be elevated in non-cancerous conditions and not elevated in some early cancers. The goal of these tests is to confirm the presence of a tumor, determine its size and location, and see if it has spread. Early detection is the single most important factor in improving survival, as it opens up the possibility of surgical removal, the only potentially curative treatment. Understanding the full spectrum of pancreatic cancer symptoms and early warning signs is a fundamental step in that early detection process.
Frequently Asked Questions
What is the most common early symptom of pancreatic cancer?
There is no single universal early symptom, but painless jaundice (yellowing of the skin and eyes) is often an early sign for tumors in the head of the pancreas. For tumors elsewhere, unexplained weight loss or new-onset diabetes may be earlier indicators.
Can pancreatic cancer symptoms come and go?
Early on, symptoms like indigestion or mild abdominal discomfort may be intermittent. However, as the cancer progresses, symptoms typically become constant and worsen over time. Any recurrent digestive issue should be evaluated.
How long do symptoms appear before diagnosis?
Symptoms often appear months before diagnosis, but they are usually subtle and attributed to other causes. The interval can vary widely, which is why awareness and prompt action are so critical.
Are pancreatic cancer symptoms different in men and women?
The core symptoms are generally the same for both sexes. However, some studies suggest women may more frequently report depression or nausea as early signs, while men may report weight loss or back pain. These differences are subtle and not reliable for diagnosis.
If I have these symptoms, does it mean I have pancreatic cancer?
No. Most people with these symptoms have far less serious conditions, such as gallstones, pancreatitis, peptic ulcers, or liver disease. The purpose of recognizing these signs is not to self-diagnose cancer, but to know when to seek professional medical evaluation to find the cause.
The journey from noticing symptoms to receiving a diagnosis can be challenging, but knowledge provides power. Recognizing the potential signs of pancreatic cancer, understanding their context, and taking swift action are the most effective tools currently available to change the trajectory of this disease. Share this information with loved ones, especially those in higher-risk categories. By fostering awareness, we can collectively work towards earlier diagnoses and better outcomes for those facing pancreatic cancer.