Osteoarthritis Pathophysiology: What Happens Inside Your Joints
Osteoarthritis (OA) is the most prevalent form of arthritis, affecting over 32.5 million adults in the United States alone. It’s often referred to as the “wear and tear” disease, but this simplistic view ignores the complex pathophysiological mechanisms behind the condition. As the population ages and obesity rates rise, the incidence of OA is expected to continue increasing globally in 2025 and beyond. Understanding the Osteoarthritis Pathophysiology is crucial for effective treatment and prevention strategies.
Understanding Osteoarthritis Pathophysiology
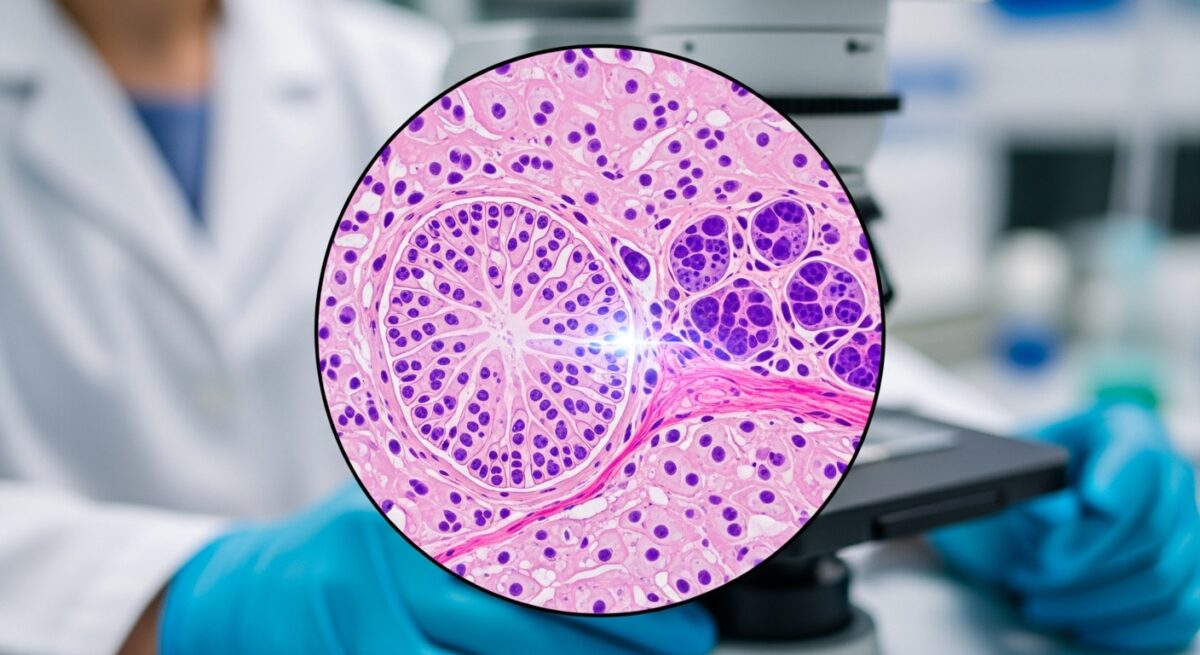
Osteoarthritis pathophysiology refers to the biological and structural changes occurring in the joint that lead to the clinical symptoms of OA. It’s a disease of the whole joint, involving cartilage, bone, synovium, ligaments, and muscles. While once considered a purely mechanical issue, recent research underscores its inflammatory and biochemical nature.
The Role of Cartilage Degradation
Articular cartilage is the smooth tissue covering the ends of bones in a joint. In OA, cartilage breakdown is a hallmark feature. Chondrocytes, the only cells in cartilage, undergo apoptosis (cell death) due to mechanical stress and inflammatory cytokines like IL-1β and TNF-α. This leads to the loss of proteoglycans and collagen type II, crucial components of healthy cartilage.
Synovial Inflammation and Its Impact
Synovitis, or inflammation of the synovial membrane, plays a pivotal role in OA progression. Synovial cells release matrix metalloproteinases (MMPs) and aggrecanases, which degrade the extracellular matrix. Inflammatory mediators not only worsen cartilage degradation but also contribute to joint pain and swelling, a common OA symptom.
Subchondral Bone Remodeling
Beneath the cartilage lies subchondral bone, which undergoes significant changes in OA. Initially, it becomes sclerotic (denser) due to microfractures and abnormal bone turnover. Over time, this leads to a stiffer joint surface, reducing shock absorption and accelerating cartilage loss.
Osteophyte Formation
Osteophytes, or bone spurs, are bony projections that form around joint margins. They develop due to altered mechanical stress and bone remodeling signals. While they may provide temporary stability, they also limit joint motion and can contribute to pain and stiffness.
Molecular Mechanisms Involved
The molecular basis of osteoarthritis involves several key pathways:
-
NF-κB pathway activation promotes inflammation
-
Wnt/β-catenin signaling affecting bone remodeling
-
MAPK signaling driving chondrocyte apoptosis
-
Elevated proinflammatory cytokines and decreased growth factors like TGF-β
Understanding these mechanisms provides targets for novel therapies in 2025 and beyond.
Risk Factors Influencing Osteoarthritis Pathophysiology
Osteoarthritis doesn’t affect everyone equally. Multiple intrinsic and extrinsic factors influence its onset and severity.
Genetic Predisposition
OA has a strong hereditary component. Studies show specific gene variants in COL2A1, GDF5, and ASPN increase susceptibility to cartilage degeneration. Epigenetic changes also influence gene expression, altering inflammatory and repair responses.
Aging and Joint Wear
Aging is a primary risk factor. As we age, cartilage loses its elasticity, and chondrocyte function declines. The ability to repair joint tissues diminishes, increasing the likelihood of OA development even without injury.
Obesity and Mechanical Stress
Excess weight adds mechanical stress to load-bearing joints like the knees and hips. Adipose tissue also acts as an endocrine organ, releasing proinflammatory cytokines (adipokines) that accelerate cartilage breakdown.
Trauma and Joint Injury
Previous joint injuries, such as meniscal tears or ligament damage, disrupt joint biomechanics. This increases cartilage wear and synovial inflammation, leading to post-traumatic osteoarthritis.
Clinical Manifestations of Osteoarthritis
The pathophysiological changes translate into a spectrum of clinical signs:
-
Joint pain worsened by activity
-
Morning stiffness lasting <30 minutes
-
Crepitus (grating sensation)
-
Decreased range of motion
-
Joint swelling and deformities (especially in late-stage)
These symptoms typically start gradually and progress over time.
Diagnostic Tools to Assess Pathophysiological Changes
Accurate diagnosis requires correlating clinical findings with imaging and lab tests:
-
X-rays reveal joint space narrowing, osteophytes, and subchondral sclerosis.
-
MRI detects early cartilage and soft tissue changes.
-
Ultrasound visualizes synovial inflammation.
-
Synovial fluid analysis rules out other types of arthritis.
Stages of Osteoarthritis Progression
OA progression is classified into stages:
-
Stage 0: Normal joint
-
Stage 1: Minor wear; possible osteophytes
-
Stage 2: Noticeable symptoms, cartilage thinning
-
Stage 3: Moderate cartilage loss, joint inflammation
-
Stage 4: Severe pain, significant cartilage, and bone damage
Understanding these stages helps guide personalized treatment plans.
Modern Approaches to Managing Osteoarthritis
Managing OA requires a multidisciplinary approach targeting symptoms and underlying pathophysiology.
Pharmacological Treatments
-
NSAIDs: Reduce inflammation and pain
-
Corticosteroids: Temporarily relieve inflammation
-
Hyaluronic acid injections: Improve joint lubrication
-
DMOADs (Disease Modifying OA Drugs): Under clinical trials for cartilage protection
Lifestyle Modifications
-
Weight loss: Significantly reduces joint load
-
Anti-inflammatory diets: Include omega-3 fatty acids and antioxidants
-
Supplements: Glucosamine and chondroitin sulfate (evidence is mixed)
Physical Therapy and Exercise
Strengthening muscles around the joint enhances stability and function. Low-impact activities like swimming, yoga, and walking are beneficial.
Surgical Interventions
In advanced OA:
-
Arthroscopy: Minimally invasive for mild cases
-
Osteotomy: Bone realignment
-
Joint replacement (arthroplasty): Common in end-stage OA
Emerging Research in Osteoarthritis Pathophysiology (2025 UPDATE)
2025 marks significant progress in OA research:
-
Regenerative medicine: Stem cells and platelet-rich plasma (PRP) show promise in cartilage regeneration.
-
Gene editing (CRISPR): Potential to silence harmful genes like MMPs
-
Targeted biologics: Aim to neutralize specific cytokines like IL-6 and TNF-α
-
Artificial intelligence in imaging: Helps detect early OA changes for preventive strategies
Leading academic sources like NIAMS provide continuous updates on these innovations.
FAQs
What is the pathophysiology of osteoarthritis?
It involves the degradation of cartilage, inflammation of the synovium, remodeling of subchondral bone, and formation of osteophytes, driven by mechanical stress and inflammatory mediators.
What is osteoarthritis pathophysiology easy?
Osteoarthritis pathophysiology means how joint damage happens. Cartilage wears down, bones change, and inflammation causes pain and stiffness.
Is osteoarthritis an inflammatory disease?
Yes, although not as strongly as rheumatoid arthritis, OA involves low-grade chronic inflammation, especially in the synovium.
How does cartilage break down in osteoarthritis?
Chondrocytes die, and enzymes like MMPs break down collagen and proteoglycans in the cartilage.
What causes osteophytes in OA?
Osteophytes form as the body tries to stabilize the joint by producing new bone where cartilage is lost.
Can osteoarthritis be reversed?
Currently, OA can’t be reversed, but symptoms can be managed, and progression can be slowed with the right interventions.
Final Thoughts
Understanding the pathophysiology of osteoarthritis is no longer limited to cartilage wear. It’s a multifaceted process involving inflammation, bone changes, and biochemical imbalances. The latest 2025 insights highlight promising treatments aimed at not just managing symptoms but targeting the root mechanisms of OA. By staying informed and integrating new therapies, patients and clinicians can work together for better outcomes and improved quality of life.
Finding the right Medicare plan shouldn’t be hard—get started now at NewMedicare.com or call 📞 (833) 203-6742!