Mouth Cancer Symptoms: Early Signs You Should Not Ignore
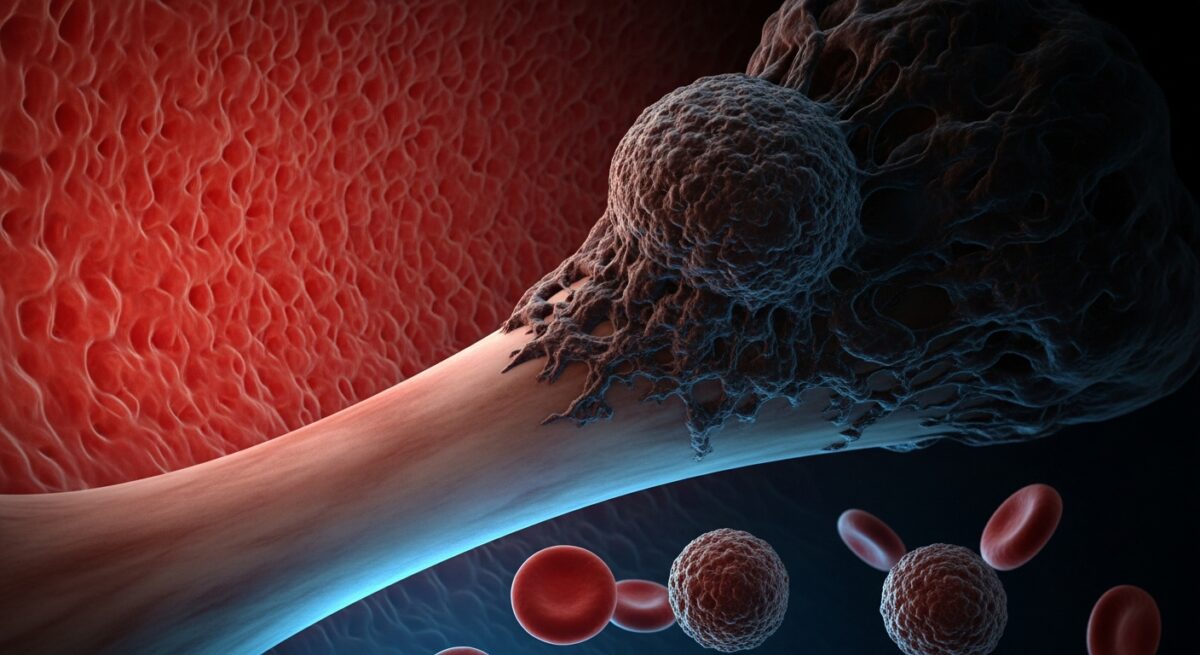
Mouth cancer, also known as oral cancer, can develop without obvious pain in its earliest stages, making awareness of its subtle symptoms a critical first line of defense. This malignancy can affect any part of the oral cavity, including the lips, tongue, cheeks, floor of the mouth, hard and soft palate, sinuses, and throat. Understanding the visual and physical changes that signal potential trouble is the key to seeking timely medical evaluation, which dramatically improves treatment outcomes. While some signs may be caused by less serious conditions, any persistent change in your mouth warrants professional attention. This guide details the specific symptoms to watch for, explains risk factors, and outlines the crucial steps to take if you notice something unusual.
Primary Symptoms and Warning Signs
The most common indicators of oral cancer are often visible or can be felt. Unlike a typical canker sore or minor irritation that heals within two weeks, precancerous and cancerous changes tend to persist. A key rule is to monitor any sore or abnormality that does not improve within 14 days. The following list outlines the primary physical symptoms that should prompt a visit to a dentist or doctor.
- A sore that does not heal: The most frequent sign is an ulcer or sore on the lip or inside the mouth that bleeds easily and does not heal within two weeks.
- Patches inside the mouth: Look for persistent red, white, or speckled (red and white) patches on the gums, tongue, tonsils, or lining of the mouth. These are known as erythroplakia and leukoplakia.
- A lump or thickening: Any lump, thickening, rough spot, crust, or small eroded area in the oral cavity or on the lip can be a warning sign.
- Unexplained numbness or pain: Persistent pain, tenderness, or numbness anywhere in the mouth, on the lip, or in the face without a clear cause.
- Difficulty with basic functions: Problems chewing, swallowing, speaking, or moving the jaw or tongue. A feeling that something is caught in the back of the throat is also notable.
These symptoms can appear individually or in combination. For instance, a red patch (erythroplakia) might develop alongside a sensation of thickness in that area of the mouth. It is important to perform regular self-examinations using a bright light and mirror to check all areas of your mouth, including under the tongue. Early detection is paramount, as localized mouth cancer has a significantly higher survival rate than cancer that has spread. Similar vigilance is required for other cancers, as detailed in our resource on recognizing uterine cancer symptoms for early detection.
Secondary Symptoms and Associated Changes
Beyond the primary localized signs, mouth cancer can cause a range of secondary symptoms that affect overall health and daily life. These often develop as the cancer progresses but can sometimes be presenting features. Persistent hoarseness or a chronic sore throat that does not resolve is a common symptom, especially for cancers affecting the oropharynx. You may experience a noticeable change in your voice, or it may sound consistently raspy. Another significant sign is a feeling of chronic ear pain, which occurs because nerves serving the face and mouth also connect to the ears. This pain is typically felt on one side only.
Unexplained weight loss is a systemic symptom that can accompany many cancers, including oral cancer, as eating may become difficult or painful. Loose teeth or dentures that suddenly no longer fit properly can indicate a tumor affecting the jawbone or gums. Finally, bad breath that persists despite good oral hygiene can be associated with tissue necrosis from a growing tumor. If you experience any of these secondary symptoms alongside a primary sign, it further underscores the urgency for a medical evaluation.
Risk Factors and Causes
Understanding what increases your risk for mouth cancer can help you make informed lifestyle choices and be more vigilant about screening. The leading cause is tobacco use in all forms, including cigarettes, cigars, pipes, chewing tobacco, and snuff. When combined with heavy alcohol consumption, the risk multiplies significantly. The human papillomavirus (HPV), particularly HPV16, is a growing cause of oropharyngeal cancers affecting the back of the throat, base of the tongue, and tonsils. This virus is distinct from the strains that cause cervical cancer.
Excessive sun exposure to the lips increases the risk of lip cancer. A personal history of any cancer, a family history of oral cancer, and a weakened immune system are also contributing factors. Poor nutrition, specifically a diet low in fruits and vegetables, may play a role. While these factors increase risk, it is crucial to remember that mouth cancer can develop in individuals with no known risk factors. This underscores why symptom awareness, not just risk profile, is essential for everyone.
The Diagnostic Process and Next Steps
If you notice a persistent symptom, your first step should be to schedule an appointment with your dentist or primary care physician. They will conduct a thorough visual and physical examination of your head, neck, and oral cavity. If they identify an area of concern, the next step is typically a biopsy. During a biopsy, a small sample of tissue is removed from the suspicious area and sent to a pathology lab for analysis. This is the only definitive way to diagnose cancer.
If the biopsy confirms cancer, further imaging tests like CT scans, MRIs, or PET scans will be used to determine the stage of the cancer, which indicates its size and whether it has spread to lymph nodes or other parts of the body. Staging guides the treatment plan. Treatment options for mouth cancer often involve surgery to remove the tumor, followed by radiation therapy and/or chemotherapy. A multidisciplinary team including surgeons, oncologists, dentists, and nutritionists is usually involved in care. Early-stage diagnosis often allows for less extensive treatment and better functional outcomes, preserving speech and swallowing ability. The diagnostic journey for blood cancers involves similar steps of vigilance and testing, as explored in our article on recognizing blood cancer symptoms for early diagnosis.
Frequently Asked Questions
Can mouth cancer be painless in the early stages?
Yes, early mouth cancer is often painless. This is why visual changes like patches or sores are so important to recognize, even if they do not hurt.
How can I tell the difference between a canker sore and mouth cancer?
A canker sore is typically painful from the start and heals completely within 10-14 days. A cancerous sore often persists beyond two weeks, may bleed, and is not always painful initially.
Who should get screened for mouth cancer?
The American Dental Association recommends that dentists perform a visual oral cancer screening as part of every routine dental checkup. Adults, especially those with risk factors, should ensure they have regular dental visits.
Does HPV cause mouth cancer?
Yes, HPV is a leading cause of oropharyngeal cancers, which affect areas like the base of the tongue and tonsils. These cancers are often located in areas not easily seen during a self-exam.
What is the survival rate for mouth cancer?
Survival rates are highly dependent on the stage at diagnosis. The five-year survival rate for localized oral cancer is around 85%, but it drops significantly if the cancer has spread to distant parts of the body. This stark difference highlights the life-saving importance of early detection.
Your oral health is a window to your overall wellbeing. Paying attention to changes in your mouth is a simple yet powerful form of self-care. Do not dismiss a persistent sore, patch, or lump. Schedule an appointment with a healthcare professional for any abnormality that lasts more than two weeks. Early action is the single most effective step you can take. Remember, you are your own best advocate when it comes to noticing the early signs of change.