Key Signs of Pancreatic Cancer: Symptoms and Early Detection
Pancreatic cancer is often called a silent disease because its early signs can be subtle, easily mistaken for more common ailments. This very lack of distinctive early warning signs contributes to its reputation for being frequently diagnosed at an advanced stage, when treatment options are more limited. Understanding the potential symptoms, even those that seem vague, is a critical step in advocating for your health. While these signs do not automatically mean cancer, recognizing them and discussing persistent changes with a healthcare provider can lead to earlier investigation and diagnosis, which is crucial for improving outcomes.
The Challenge of Early Detection
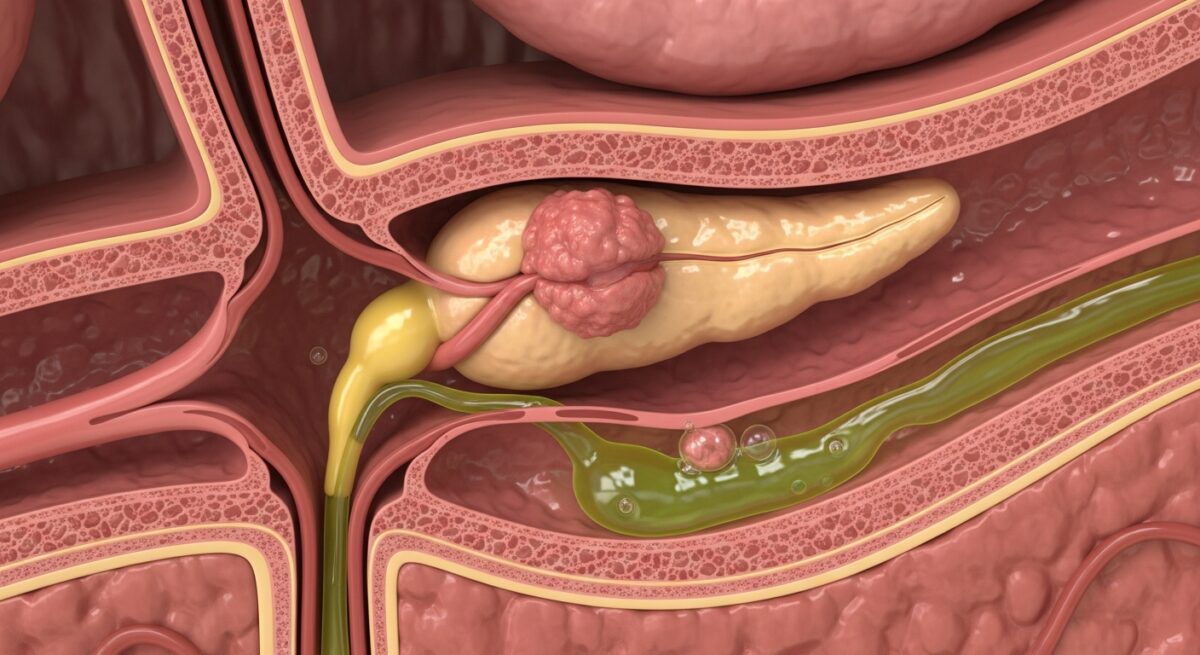
One of the primary reasons pancreatic cancer carries a significant mortality rate is the organ’s hidden location deep within the abdomen, behind the stomach. A small tumor here typically causes no initial pain or noticeable symptoms. Furthermore, many of the early signs are nonspecific, overlapping with symptoms of conditions like irritable bowel syndrome, gastritis, or chronic pancreatitis. This ambiguity often leads to a delay in seeking medical attention or in receiving the correct diagnostic tests. It is the persistence, combination, and worsening of these symptoms that often raise the first red flags for clinicians.
Common Signs and Symptoms
The manifestations of pancreatic cancer can vary depending on the tumor’s location within the pancreas (head, body, or tail) and whether it is affecting specific nearby structures. Symptoms generally fall into two categories: those caused by the tumor’s local presence and those resulting from the cancer’s effect on the body’s systems. A comprehensive look at pancreatic cancer symptoms and early warning signs can provide a deeper understanding of this progression.
Jaundice: A Telltale Sign
Jaundice is one of the most recognizable signs, particularly for tumors located in the head of the pancreas, which is close to the common bile duct. When a tumor blocks this duct, bile cannot drain properly from the liver into the intestine. This backup causes a yellowish pigment called bilirubin to build up in the bloodstream. The resulting jaundice presents as a yellowing of the skin and the whites of the eyes. It is often accompanied by other distinct changes.
Key indicators of obstructive jaundice include:
- Dark urine: The excess bilirubin is excreted through the kidneys, making urine the color of tea or cola.
- Light-colored or greasy stools: Without bile acids reaching the intestines, stools lose their normal brown color and can become pale, gray, or clay-colored. The lack of bile also impairs fat digestion, leading to stools that are oily, float, and are unusually foul-smelling (steatorrhea).
- Itchy skin: The buildup of bilirubin salts under the skin can cause persistent, generalized itching.
It is important to note that jaundice is a medical symptom that always requires prompt evaluation. While it can be caused by other conditions like gallstones or hepatitis, its association with pancreatic cancer makes immediate investigation essential.
Abdominal and Back Pain
Pain is a common but often later-developing symptom. It typically originates in the upper abdomen and may radiate to the mid or upper back. This pain pattern occurs because the pancreas is located in front of the spine; as a tumor grows, it can press on nerves in the surrounding area. The character of the pain is often described as a dull ache or a feeling of pressure that may come and go initially but tends to become more constant and severe over time. It might worsen after eating or when lying down, and some people find partial relief by leaning forward. This type of persistent, unexplained abdominal and back pain, especially in someone without a history of back problems, warrants medical attention.
Systemic and Digestive Symptoms
Beyond localized signs, pancreatic cancer often causes a range of broader systemic symptoms that affect overall health and digestion. These can be the most insidious, as they are easily attributed to stress, aging, or other minor illnesses.
Unexplained Weight Loss and Appetite Changes
Significant, unintentional weight loss is a hallmark of many cancers, including pancreatic cancer. This occurs through a combination of factors. The cancer itself alters the body’s metabolism, increasing calorie expenditure even at rest. Furthermore, digestive symptoms like nausea or early satiety (feeling full after eating only a small amount) can lead to reduced food intake. Crucially, when the pancreas is not functioning properly, it may not produce enough digestive enzymes to break down food, leading to malabsorption of nutrients. This means even if a person is eating, their body cannot properly absorb the calories and nutrients from the food.
Nausea, Vomiting, and Digestive Issues
When a tumor presses on the far end of the stomach (the duodenum), it can partially block the passage of food, causing a feeling of fullness, nausea, and vomiting, especially after meals. This obstruction can lead to cyclical vomiting of undigested food. As mentioned, the loss of pancreatic enzymes leads to poor digestion, particularly of fats, resulting in bloating, gas, and the steatorrhea described earlier. These persistent digestive upsets, particularly when new and not linked to a specific dietary change, are important to discuss with a doctor.
New-Onset Diabetes and Other Warning Signs
Sometimes, pancreatic cancer reveals itself through seemingly unrelated health changes. Two particularly important ones are new-onset diabetes and blood clot formation.
The pancreas produces insulin, which regulates blood sugar. A tumor can damage insulin-producing cells, leading to insulin resistance or deficiency. Therefore, the development of type 2 diabetes in someone over age 50 with a healthy weight and no family history is a potential red flag that requires thorough evaluation. Similarly, a sudden, unexplained episode of venous thromboembolism (a blood clot in a deep vein, often in the leg, or a pulmonary embolism in the lung) can sometimes be the first sign of an underlying cancer, including pancreatic cancer. Cancers can produce substances that make the blood more prone to clotting.
Other general symptoms include profound fatigue that doesn’t improve with rest, depression (which may be both a reaction to other symptoms and a biological effect of the cancer), and a general sense of being unwell. For a detailed breakdown of what specific symptoms to watch for and their implications, our resource on pancreatic cancer symptoms offers further guidance.
Risk Factors and When to See a Doctor
Understanding personal risk can help contextualize symptoms. Major risk factors include smoking, chronic pancreatitis, long-standing diabetes, a family history of pancreatic cancer or certain genetic syndromes (like BRCA mutations), obesity, and older age (most cases occur after 65). Having one or more risk factors does not mean you will get cancer, but it may mean you should be more vigilant about symptoms.
The key message is to seek medical evaluation for persistent symptoms. “Persistent” generally means a symptom that lasts for more than two weeks without a clear explanation or that is worsening over time. Be prepared to describe your symptoms in detail: when they started, their character, what makes them better or worse, and how they are affecting your daily life. Given the complexity of health coverage for such diagnostics, it’s wise to understand your insurance benefits. For those on Medicare, exploring the details of Read full article about coverage for cancer screenings and specialist visits is a prudent step.
Frequently Asked Questions
What is usually the first symptom of pancreatic cancer?
There is no single “first” symptom that applies to everyone. For tumors in the head of the pancreas, painless jaundice is often an early sign. For tumors in the body or tail, unexplained weight loss, dull abdominal pain radiating to the back, or new-onset diabetes may be the initial clues. The onset is often gradual.
How can I check for pancreatic cancer at home?
You cannot diagnose pancreatic cancer at home. There is no self-exam. The most important action you can take is to be aware of your body and note any persistent changes in the signs discussed, such as jaundice, pain, weight loss, or digestive issues, and report them promptly to a healthcare professional for proper evaluation.
Where is pancreatic cancer pain felt?
Pain is most commonly felt in the upper abdomen, just below the breastbone. It frequently bores through to the mid-back or upper back. The pain may be intermittent at first and become constant, often worsening after meals or when lying flat.
Is pancreatic cancer curable if caught early?
Early detection dramatically improves the prognosis. When pancreatic cancer is found at a very early, localized stage (before it has spread), surgical removal offers the best chance for a cure. However, because early-stage disease often lacks symptoms, these cases are less common. This underscores the critical importance of investigating potential warning signs.
Recognizing the signs of pancreatic cancer is an act of health empowerment. While the thought of this disease is frightening, knowledge provides a measure of control. Do not dismiss persistent changes in your body as insignificant. By acting as your own advocate, documenting symptoms, and seeking timely medical consultation, you ensure that any potential issue is investigated appropriately. Early intervention remains the most powerful tool in improving outcomes for pancreatic cancer and many other serious health conditions.