Key Signs of Cervical Cancer and Early Warning Symptoms
Cervical cancer often develops silently, with subtle signs that can be easily overlooked or mistaken for other common conditions. Understanding these potential warning signals is a critical step in protecting your health, as early detection dramatically improves treatment outcomes. This guide details the specific symptoms that may indicate cervical cancer, explains what they mean, and underscores the vital importance of regular screening, which can identify precancerous changes before they ever develop into cancer.
Understanding Cervical Cancer and Its Progression
Cervical cancer begins in the cells lining the cervix, the lower part of the uterus that connects to the vagina. Nearly all cases are caused by persistent infection with certain high risk strains of the human papillomavirus (HPV). The body’s immune system typically clears HPV naturally, but when the infection persists, it can cause changes to cervical cells over many years. These changes progress from precancerous conditions, known as dysplasia or cervical intraepithelial neoplasia (CIN), to invasive cancer. This slow progression is precisely why regular Pap tests and HPV tests are so powerful, they can catch these cellular changes long before a woman experiences a single symptom. Recognizing the later signs, however, is equally crucial for those who may have fallen behind on screening.
The Most Common Signs and Symptoms of Cervical Cancer
Early stage cervical cancer frequently causes no signs at all. When symptoms do appear, they often mimic other less serious issues, which is why they are frequently dismissed. It is essential to consult a healthcare provider if you experience any of the following, especially if they are new, persistent, or worsening. A deeper exploration of these cervical cancer symptoms and early warning signs can provide further context for understanding their significance.
Abnormal Vaginal Bleeding
This is the most common and often the first noticeable symptom of cervical cancer. It refers to any bleeding that occurs outside of your normal menstrual period. Key patterns to watch for include bleeding after sexual intercourse (postcoital bleeding), bleeding after menopause, bleeding between regular menstrual periods, and menstrual periods that are heavier or last longer than usual. Any postmenopausal bleeding warrants immediate medical evaluation, as it is never considered normal.
Unusual Vaginal Discharge
An increase in vaginal discharge or a change in its characteristics can be a sign. The discharge may be watery, pink, or brown tinged (often described as “watery, bloody discharge”). It may have a foul or unpleasant odor. While discharge can vary normally due to hormonal cycles or infections, a persistent, new change that doesn’t resolve should be investigated.
Pelvic Pain or Pain During Intercourse
Pain is generally a later sign, indicating the cancer may be growing into surrounding tissues. This can manifest as pelvic pain not related to your menstrual cycle, pain during or after sexual intercourse (dyspareunia), or a persistent dull ache in the lower back or pelvis. This pain differs from typical menstrual cramps and is often more constant.
Advanced Symptoms and When Cancer Spreads
If cervical cancer grows and spreads (metastasizes) to other parts of the body, it can cause additional, more generalized symptoms. These indicate a more advanced stage and require urgent medical attention.
- Urinary Problems: Difficulty urinating, pain during urination, or blood in the urine if the cancer affects the bladder.
- Leg Swelling: Swelling in one or both legs can occur if the cancer blocks lymphatic vessels or blood flow.
- Kidney Failure: Advanced tumors can block the ureters (tubes from kidneys to bladder), leading to kidney failure, which may cause nausea, vomiting, and loss of appetite.
- Weight Loss and Fatigue: Unexplained weight loss and extreme, persistent fatigue are common in many advanced cancers as the body’s resources are depleted.
It is critical to remember that these symptoms are not exclusive to cervical cancer and are more often caused by benign conditions like infections, fibroids, or hormonal fluctuations. However, their presence, especially in combination, is a clear signal that you need a professional evaluation to determine the cause.
Risk Factors and the Role of HPV
Knowing the signs is only one part of the equation. Understanding your personal risk factors helps contextualize your vigilance. The primary risk factor is persistent infection with a high risk HPV type (especially HPV 16 and 18). Other factors that increase risk include smoking, which weakens the immune system’s ability to fight HPV, having a weakened immune system (from conditions like HIV or immunosuppressive medications), long term use of oral contraceptives (though the risk decreases after stopping), and having multiple full term pregnancies. A family history of cervical cancer may also play a role. Importantly, the HPV vaccine is a highly effective preventive tool against the strains that cause most cervical cancers. It is recommended for preteens but can be given through age 45. Our dedicated guide on recognizing cervical cancer symptoms and early warning signs discusses how these risk factors interact with symptom presentation.
Screening and Prevention: Your Best Defense
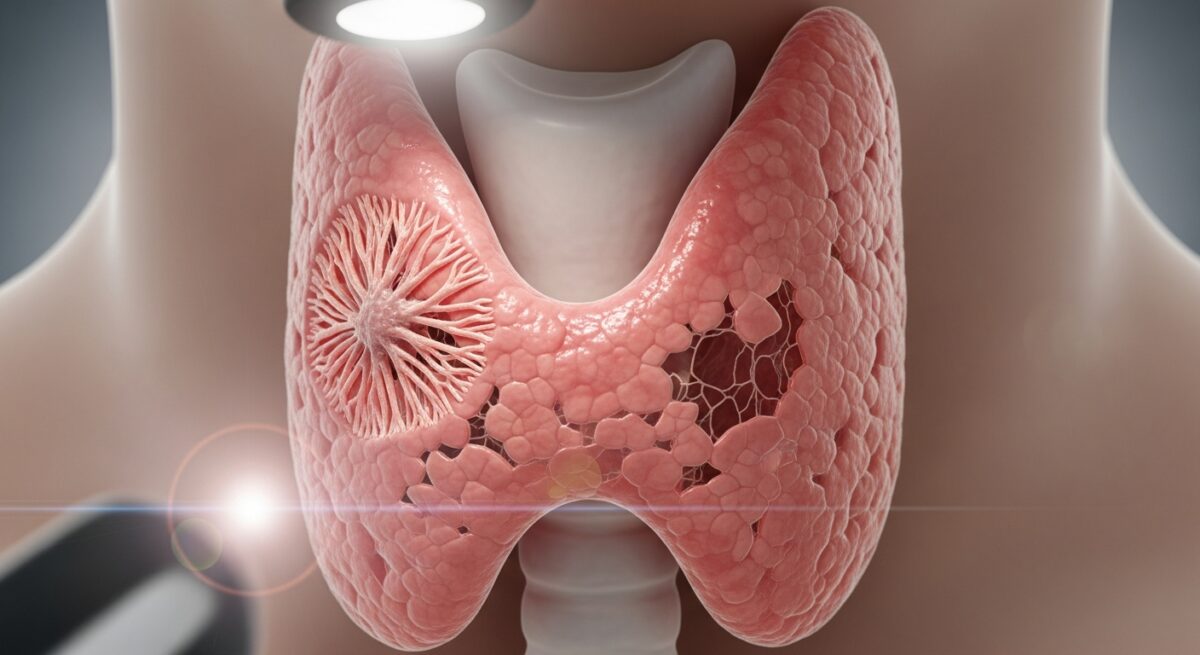
Screening is the cornerstone of cervical cancer prevention. It aims to find precancerous cell changes before they turn into cancer. The two main tests are the Pap test (or Pap smear) and the HPV test. A Pap test collects cells from the cervix to look for abnormalities. An HPV test checks for the presence of the virus itself. Current guidelines recommend that women begin screening at age 21. The interval between tests (every 3 or 5 years) depends on your age and whether you are having a Pap test alone or a Pap/HPV co test. Adhering to these guidelines is the single most effective action you can take. If screening detects abnormalities, follow up procedures like a colposcopy (a magnified examination of the cervix) and possibly a biopsy will be recommended to obtain a definitive diagnosis.
Frequently Asked Questions
At what age do cervical cancer symptoms typically appear?
Cervical cancer is most frequently diagnosed in women between the ages of 35 and 44. Symptoms can appear at any age after the cancer has developed, but because it progresses slowly, symptoms in women under 20 are extremely rare.
Can you have cervical cancer with no symptoms?
Absolutely. Early stage cervical cancer and precancerous conditions often produce no symptoms whatsoever. This is why routine screening is non negotiable, it detects problems before symptoms arise.
How long can you have cervical cancer without knowing?
It is possible to have precancerous changes or very early stage cancer for years without any signs. The progression from HPV infection to cancer typically takes 10 to 20 years, providing a long window for screening to intercept it.
What should I do if I’m experiencing possible signs?
Schedule an appointment with your gynecologist or primary care provider immediately. Do not wait for your next scheduled screening. Be prepared to describe your symptoms in detail, including when they started, their frequency, and any patterns you’ve noticed.
Are the signs of cervical cancer different from ovarian or uterine cancer?
Yes, there can be overlap (like abnormal bleeding), but each has distinct patterns. Cervical cancer is more uniquely associated with bleeding after sex. Ovarian cancer symptoms are often vague (bloating, feeling full quickly). Uterine cancer most commonly causes postmenopausal bleeding. A doctor can perform the appropriate exams to differentiate.
Being informed about the signs of cervical cancer empowers you to take an active role in your health. While this information is vital, it is not a substitute for professional medical advice or regular screening. If you notice any persistent changes in your body, particularly abnormal bleeding or discharge, prioritize a conversation with your healthcare provider. Early action is the key to successful treatment and long term health.