Gallbladder Cancer: Symptoms, Risk Factors, and Treatment Options
Gallbladder cancer is a rare but serious malignancy that begins in the tissues of the gallbladder, a small, pear-shaped organ beneath the liver. Its rarity and often silent progression present significant challenges, as symptoms frequently appear only in advanced stages. Understanding this disease, its subtle warning signs, and the factors that increase risk is crucial for early detection and effective management. This comprehensive guide provides an in-depth look at gallbladder cancer, empowering patients and families with essential knowledge.
Understanding Gallbladder Cancer and Its Development
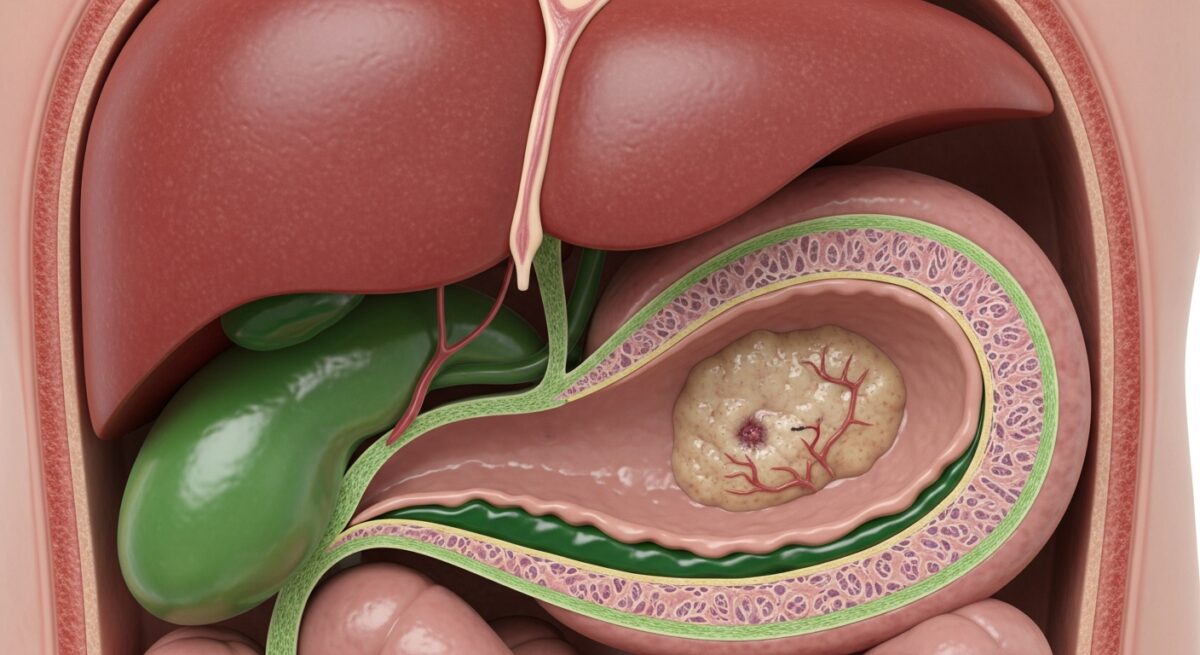
The gallbladder’s primary function is to store and concentrate bile, a digestive fluid produced by the liver. Cancer arises when cells in the gallbladder’s lining begin to grow uncontrollably. The most common type is adenocarcinoma, which starts in the glandular cells that line the inner surface of the gallbladder. Due to the organ’s small size and location, cancer can grow undetected for some time and may spread to nearby structures like the liver, bile ducts, and lymph nodes. This pattern of late discovery contributes to the disease’s overall poor prognosis compared to other cancers. The staging of gallbladder cancer, from Stage 0 (carcinoma in situ) to Stage IV (distant spread), directly influences treatment strategy and outlook.
Recognizing the Symptoms and Signs
Early-stage gallbladder cancer often causes no noticeable symptoms. When symptoms do occur, they can be vague and easily mistaken for more common conditions like gallstones or indigestion. This ambiguity is why awareness is critical. The most common symptom is abdominal pain, typically in the upper right quadrant. Other signs may include jaundice (yellowing of the skin and eyes), which occurs when a tumor blocks the bile ducts, unexplained weight loss, nausea and vomiting, and bloating. A palpable lump in the abdomen and fever may also be present. It is vital to consult a healthcare provider if any of these symptoms persist, especially if you have known risk factors. Persistent symptoms warrant investigation beyond simple explanations.
Key Risk Factors and Causes
While the exact cause of gallbladder cancer is not fully understood, several factors significantly increase an individual’s risk. The most prominent risk factor is a history of gallstones and chronic inflammation of the gallbladder (cholecystitis). However, it is important to note that while gallstones are very common, gallbladder cancer is very rare. Other important risk factors include gallbladder polyps (especially those larger than 1 centimeter), porcelain gallbladder (a condition where the gallbladder wall becomes calcified), female gender, older age (most common in people over 65), and certain ethnicities (higher rates are seen in Native American and Mexican populations).
Additional elements linked to increased risk include:
- Primary Sclerosing Cholangitis: A disease causing inflammation and scarring of the bile ducts.
- Congenital Bile Duct Abnormalities: Such as choledochal cysts.
- Obesity: Which increases the risk of gallstone formation.
- Exposure to Certain Chemicals: Found in industrial settings, like those used in rubber and textile manufacturing.
Understanding these risks can guide conversations with a doctor about surveillance or preventive measures, such as the removal of the gallbladder (cholecystectomy) for high-risk conditions like large polyps.
Diagnostic Procedures and Staging
Diagnosing gallbladder cancer typically begins with a physical exam and a review of medical history. If cancer is suspected, a series of tests will be ordered to confirm the diagnosis and determine the extent, or stage, of the disease. Imaging tests are fundamental. An abdominal ultrasound is often the first test, as it can visualize gallstones, polyps, and masses. A CT scan provides detailed cross-sectional images to assess the tumor size and potential spread. An MRI, particularly an MRCP (Magnetic Resonance Cholangiopancreatography), offers excellent views of the bile ducts, liver, and pancreas.
For a definitive diagnosis, a biopsy is usually required. This involves removing a small sample of tissue for examination under a microscope. This can sometimes be done with a fine needle guided by ultrasound or CT. Blood tests may also reveal liver function abnormalities or elevated tumor markers like CA 19-9. Once diagnosed, staging tests (which may include specialized scans like a PET scan) determine if and where the cancer has spread. Accurate staging is the cornerstone for developing an effective, personalized treatment plan.
Treatment Pathways and Modern Approaches
Treatment for gallbladder cancer depends heavily on the stage at diagnosis, the patient’s overall health, and personal preferences. A multidisciplinary team of specialists, including surgical oncologists, medical oncologists, and radiation oncologists, collaborates to create the best plan. Surgery offers the only potential cure for localized disease. The standard procedure is a radical cholecystectomy, which involves removing the gallbladder, a margin of healthy liver tissue, and nearby lymph nodes. For more advanced local disease, a more extensive operation may be necessary.
When surgery cannot remove all the cancer, or if the cancer has spread, other treatments become the primary focus. Chemotherapy uses drugs to kill cancer cells or stop their growth throughout the body. Radiation therapy uses high-energy beams to target and destroy cancer cells in a specific area. Often, chemotherapy and radiation are used together (chemoradiation) after surgery to kill any remaining cells, or before surgery to shrink a tumor. For advanced cancers, palliative treatments focus on relieving symptoms and improving quality of life, such as placing a stent to keep a bile duct open and relieve jaundice. Clinical trials also offer access to new therapies, including targeted drugs and immunotherapy, which are areas of active research.
Frequently Asked Questions
What is the survival rate for gallbladder cancer?
Survival rates vary widely based on the stage at diagnosis. When detected early and confined to the gallbladder, the 5-year survival rate is significantly higher. However, because many cases are found at an advanced stage, the overall 5-year survival rate is lower. It is essential to discuss individual prognosis with your oncology team, as statistics are population-based and do not predict an individual’s outcome.
Can gallbladder cancer be prevented?
There is no guaranteed way to prevent gallbladder cancer, but managing risk factors can help. Maintaining a healthy weight, eating a diet rich in fruits and vegetables, and getting regular physical activity may reduce the risk of gallstones. For individuals with high-risk conditions like large gallbladder polyps, doctors may recommend preventive gallbladder removal.
Is gallbladder cancer hereditary?
Most cases are not directly inherited. However, having a family history of gallbladder cancer does slightly increase risk, possibly due to shared genetic predispositions or environmental factors. Certain genetic syndromes are associated with a higher risk of biliary cancers, but these are rare.
What are the side effects of common treatments?
Surgery carries risks like infection, bleeding, and damage to nearby organs. Chemotherapy side effects can include fatigue, nausea, low blood counts, and hair loss. Radiation may cause skin irritation, fatigue, and nausea. Your care team will provide supportive care to manage these effects.
Where can I find support as a patient or caregiver?
Support is crucial. Seek help from hospital social workers, patient navigators, and reputable organizations like the American Cancer Society. Online and in-person support groups connect you with others who understand the journey. Don’t hesitate to ask your medical team for mental health resources as well.
Navigating a gallbladder cancer diagnosis is a profound challenge, but you are not alone. Advances in surgical techniques, systemic therapies, and supportive care continue to improve outcomes and quality of life. Being an informed advocate, asking detailed questions of your healthcare team, and building a strong support network are powerful steps on this path. Focus on the information and care options available today to make the decisions that are right for you or your loved one.