Eosinophils And Cancer: What High Levels Mean
When a routine blood test shows elevated eosinophils, it’s natural for your mind to leap to the most serious possibilities. You might find yourself searching for answers, specifically wondering what level of eosinophils indicate cancer. The relationship between these white blood cells and malignancy is complex, and while persistent, marked eosinophilia can be a red flag for certain cancers, it is far from a standalone diagnostic tool. Understanding the nuances of eosinophil counts, the context in which they occur, and the extensive differential diagnosis is crucial for interpreting your lab results and collaborating effectively with your healthcare team.
Understanding Eosinophils And Their Normal Range
Eosinophils are a type of white blood cell that play a key role in your body’s immune system. They are primarily involved in combating parasitic infections and modulating allergic and asthmatic responses. In a healthy individual, eosinophils make up a small percentage of the total white blood cell count. The normal absolute eosinophil count (AEC) typically falls between 30 and 350 cells per microliter (µL) of blood. This represents about 0% to 6% of your total white blood cells. It is important to note that reference ranges can vary slightly between different laboratories. A result outside this range is called eosinophilia, which is categorized by severity: mild (351-1500 cells/µL), moderate (1500-5000 cells/µL), and severe (greater than 5000 cells/µL). The clinical significance of an elevated count depends heavily on the degree of elevation and, more importantly, the underlying cause.
When Do Elevated Eosinophils Signal Cancer Risk?
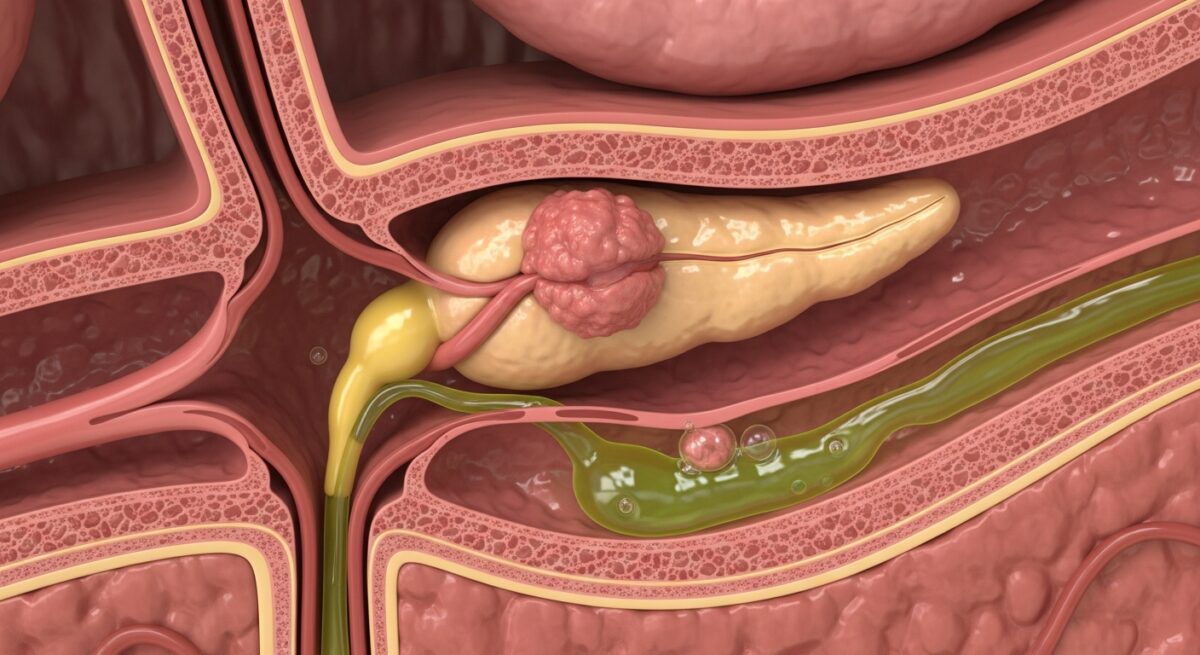
So, what level of eosinophils indicate cancer? There is no single numeric threshold that definitively points to cancer. A very high count (severe eosinophilia) certainly raises more concern and warrants a thorough investigation, but the number itself is not diagnostic. The context is everything. Cancer-related eosinophilia, known as paraneoplastic eosinophilia, occurs when a tumor stimulates the bone marrow to overproduce these cells or secretes substances that promote eosinophil growth. This phenomenon is most strongly associated with specific types of cancers. Blood cancers, particularly certain lymphomas (like Hodgkin lymphoma) and leukemias (such as acute myeloid leukemia or chronic eosinophilic leukemia), are classic culprits. Solid tumors, including those of the lung, stomach, colon, ovary, and pancreas, can also sometimes trigger eosinophilia.
The key indicator is often persistence and progression. A mild, transient elevation is common and usually benign, often linked to allergies or a passing infection. A cause for greater concern is a persistently high or rapidly rising eosinophil count that cannot be explained by more common conditions. For instance, if a patient has severe, unexplained eosinophilia that persists for months despite treatment for common triggers, and is accompanied by other systemic symptoms like unexplained weight loss, fever, night sweats, or fatigue, the suspicion for an underlying malignancy increases significantly. In such cases, the eosinophilia is a clue, a symptom of a deeper problem, not the problem itself.
The Critical Diagnostic Process Beyond The Lab Number
Focusing solely on what level of eosinophils indicate cancer misses the broader, more critical picture of diagnosis. Eosinophilia is a signpost, not a destination. The diagnostic journey when faced with significant, unexplained eosinophilia is comprehensive and methodical. The first and most crucial step is a detailed consultation with a physician, often a hematologist or an oncologist. They will take a full medical history, including travel, allergies, medication use, and a review of all symptoms. A thorough physical exam follows, checking for lymph node enlargement, skin rashes, or organ enlargement.
The laboratory workup extends far beyond the basic complete blood count (CBC). It typically includes peripheral blood smear analysis, where a technologist visually examines the blood cells for abnormalities. Additional tests aim to rule out the vast number of non-cancerous causes first. This diagnostic process is systematic.
- Exclude Common Causes: Testing for parasitic infections, assessing for allergic and autoimmune conditions (like eosinophilic granulomatosis with polyangiitis), and reviewing all medications.
- Advanced Blood and Imaging Studies: This may include tests for specific genetic mutations (e.g., FIP1L1-PDGFRA fusion gene), immunoglobulin levels, and imaging scans (CT, PET) to look for tumors or lymph node involvement.
- Tissue Biopsy: If a specific organ or lymph node is suspect, a biopsy is the gold standard for diagnosing cancer. A bone marrow biopsy and aspiration is almost always performed in cases of severe, unexplained eosinophilia to directly assess blood cell production and look for evidence of leukemia or lymphoma.
- Multidisciplinary Review: Results are synthesized by a team of specialists to arrive at a definitive diagnosis.
This exhaustive process underscores that cancer is only one of many possibilities. More often than not, investigations point to other, more prevalent conditions. For a deeper exploration of navigating complex health diagnoses and insurance coverage, you can Read full article on related healthcare topics.
Non-Cancerous Causes Of High Eosinophil Counts
It is statistically far more likely that eosinophilia is due to a cause other than cancer. The list of non-malignant conditions is extensive and should always be investigated first. Allergic disorders are the most common trigger, including asthma, hay fever (allergic rhinitis), and atopic dermatitis. Drug reactions can also provoke significant eosinophilia. Various infections, particularly parasitic infections like strongyloidiasis or ascariasis, are major causes worldwide. Autoimmune and inflammatory diseases, such as eosinophilic granulomatosis with polyangiitis (EGPA), eosinophilic esophagitis, or inflammatory bowel disease, can feature elevated eosinophils as part of their pathology. Primary eosinophilic disorders, like hypereosinophilic syndrome (HES), are conditions where eosinophils are overproduced without a clear secondary cause and can cause organ damage but are distinct from cancer. Differentiating these conditions from malignancy is the central task of the diagnostic workup.
Frequently Asked Questions
Can eosinophilia be the only sign of cancer?
It is extremely rare for eosinophilia to be the only sign. It is almost always accompanied by other symptoms, such as unexplained weight loss, persistent fever, night sweats, fatigue, lumps (enlarged lymph nodes), pain, or specific symptoms related to the organ where a tumor might be located.
What is considered a dangerously high eosinophil count?
Counts above 1,500 cells/µL (moderate eosinophilia) are considered significant and require medical evaluation. Counts persistently above 5,000 cells/µL (severe eosinophilia) are considered dangerous due to the risk of tissue damage from eosinophil infiltration, regardless of the cause, and demand urgent and thorough investigation.
If my eosinophils are high, should I see an oncologist immediately?
Not necessarily. The first step is usually to see your primary care physician. They will conduct an initial evaluation to rule out common causes. Based on their findings, the persistence of the high count, and the presence of other concerning symptoms, they may then refer you to a specialist, which could be an allergist, pulmonologist, infectious disease doctor, hematologist, or oncologist.
How is cancer-related eosinophilia treated?
Treatment is directed at the underlying cancer itself. Successful treatment of the primary tumor with surgery, chemotherapy, radiation, or targeted therapies will typically lead to the normalization of the eosinophil count. In some cases, specific therapies may be used to lower the eosinophil count directly to manage symptoms if they are causing tissue damage.
Can low eosinophils indicate cancer?
Low eosinophil counts (eosinopenia) are less commonly discussed but can occur. They are not typically a specific indicator of cancer. Low counts can be seen with acute stress, Cushing’s syndrome, or with certain treatments like corticosteroid use. They are generally not a primary diagnostic clue for malignancy.
Interpreting a high eosinophil count requires careful medical expertise and a systematic diagnostic approach. While understanding what level of eosinophils indicate cancer is a valid concern, it is vital to remember that this finding is a starting point for investigation, not a conclusion. A persistently and severely elevated count demands a thorough workup to identify the root cause, which spans a wide spectrum from common allergies to rare cancers. Partnering with your healthcare provider, providing a complete history, and undergoing the recommended tests are the only ways to move from anxiety-inducing lab results to a clear diagnosis and an appropriate treatment plan. Your vigilance and their clinical acumen together form the best defense for your health.