Bile Duct Cancer: Symptoms, Stages, and Treatment Options
Bile duct cancer, medically known as cholangiocarcinoma, is a rare but aggressive malignancy that originates in the slender tubes responsible for carrying digestive fluid from your liver to your gallbladder and small intestine. Often called the “silent” cancer due to its vague, late presenting symptoms, understanding this disease is critical for early detection and navigating the complex path to effective care, especially for those navigating healthcare coverage like Medicare.
Understanding Bile Duct Cancer and Its Types
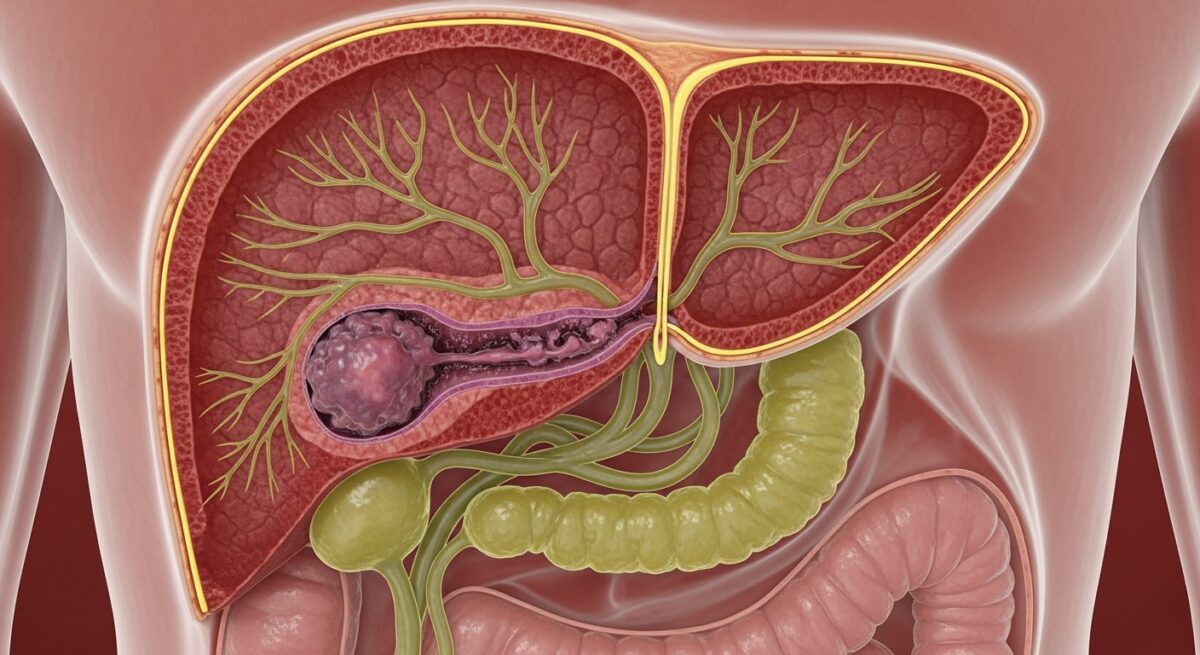
To grasp bile duct cancer, one must first understand the biliary system. The bile ducts form a branching network, a drainage system for bile produced by the liver. When cancerous cells develop in the lining of these ducts, they can obstruct bile flow, leading to jaundice (yellowing of the skin and eyes), a common first sign. Doctors classify cholangiocarcinoma based on its location within this network, which significantly influences symptoms, treatment approach, and prognosis. The three primary types are intrahepatic, perihilar, and distal cholangiocarcinoma.
Intrahepatic bile duct cancers occur within the liver itself, in the smaller ducts. They are sometimes confused with liver cancer (hepatocellular carcinoma). Perihilar cholangiocarcinoma, also known as a Klatskin tumor, develops at the hilum, where the left and right hepatic ducts join just outside the liver. This is the most common location. Distal bile duct cancers are found further down the duct, closer to where it empties into the small intestine. The location dictates the surgical options available, as removing the tumor often requires complex procedures that may involve parts of the liver, pancreas, or small intestine.
Recognizing the Symptoms and Risk Factors
Symptoms of bile duct cancer typically arise when the tumor grows large enough to block the bile ducts. Early signs are often nonspecific and easily attributed to other, less serious conditions. This delay in recognition is a major challenge. The most common symptom is jaundice, which results from the buildup of bilirubin in the blood. Other symptoms can include intense itching (pruritus), dark urine, pale or clay colored stools, unexplained weight loss, loss of appetite, fever, and abdominal pain, particularly in the upper right side.
While the exact cause of cholangiocarcinoma is not always clear, several risk factors have been identified. Primary sclerosing cholangitis (PSC), a chronic inflammatory disease of the bile ducts, is a significant risk factor. Other conditions include bile duct cysts (choledochal cysts), chronic liver disease such as cirrhosis or hepatitis B or C infection, liver fluke parasitic infections (more common in Asia), and certain inherited metabolic conditions. Age is also a factor, with most diagnoses occurring in people over 50. Understanding these risks can help individuals and their doctors maintain appropriate vigilance.
Diagnosis and Staging of Cholangiocarcinoma
Diagnosing bile duct cancer involves a multi step process, as imaging and tissue analysis are crucial. The journey often begins with blood tests to check liver function and for elevated tumor markers like CA 19 9. Imaging studies are the cornerstone of diagnosis and staging. These may include ultrasound, computed tomography (CT) scans, magnetic resonance imaging (MRI) with magnetic resonance cholangiopancreatography (MRCP), which provides detailed pictures of the bile ducts, and positron emission tomography (PET) scans to check for spread.
A definitive diagnosis usually requires a biopsy, where a small sample of tissue is removed for examination under a microscope. This can sometimes be done via endoscopic retrograde cholangiopancreatography (ERCP) or percutaneous transhepatic cholangiography (PTC), procedures that also allow for stent placement to relieve blockages. Once diagnosed, the cancer is staged to determine its extent. Staging follows the TNM system, evaluating the Tumor size and invasion, lymph Node involvement, and Metastasis (spread to distant organs). Accurate staging is vital for determining whether the cancer is potentially resectable (removable by surgery) and for guiding all subsequent treatment decisions. Navigating these complex diagnostic procedures highlights the importance of comprehensive health insurance, such as Medicare Advantage plans, which can cover a wide range of specialized tests and specialist visits. For a deeper look at coverage options for complex cancer care, you can Read full article on our dedicated health insurance resource page.
Current Treatment Options and Approaches
Treatment for bile duct cancer is highly individualized and depends primarily on the stage and location of the tumor, as well as the patient’s overall health. A multidisciplinary team including oncologists, surgeons, radiologists, and gastroenterologists is essential for crafting an effective plan. The only potential cure for localized cholangiocarcinoma is complete surgical removal. The type of surgery is major and varies: it may involve removing part of the liver (liver resection), the entire bile duct, the gallbladder, and sometimes portions of the pancreas and small intestine (a Whipple procedure).
For cancers that cannot be surgically removed (unresectable), or for cases where surgery is not an option, treatment focuses on controlling the cancer, relieving symptoms, and improving quality of life. In these situations, chemotherapy and radiation therapy are the mainstays. Chemotherapy drugs like gemcitabine and cisplatin are commonly used, either alone or in combination. Radiation therapy can help shrink tumors and alleviate blockages. Targeted therapy and immunotherapy are newer, promising areas of treatment. These drugs target specific genetic mutations or boost the body’s immune system to fight cancer cells, offering hope for patients whose cancers have specific biomarkers. Palliative care, including procedures to place stents or drains to keep bile ducts open, is a critical component of management at any stage to manage jaundice, pain, and infection.
Frequently Asked Questions About Bile Duct Cancer
What is the life expectancy for someone with bile duct cancer?
Prognosis varies widely based on stage at diagnosis, tumor location, and overall health. When detected early and surgically removed, long term survival is possible. For advanced, unresectable cancer, treatment focuses on prolonging life and managing symptoms. Five year survival rates are generally lower for this cancer type, underscoring the need for early detection.
Is bile duct cancer hereditary?
Most cases are not directly inherited. However, certain genetic syndromes that increase risk, such as Lynch syndrome, can run in families. Having a first degree relative with cholangiocarcinoma may slightly increase risk, likely due to shared environmental or genetic factors.
What are the first signs of bile duct cancer?
Jaundice (yellowing skin/eyes) is often the first noticeable sign. It may be preceded by itching, dark urine, or pale stools. Unexplained weight loss, fatigue, and mild abdominal pain are other potential early warnings.
How is bile duct cancer treated if surgery isn’t an option?
For inoperable cancer, treatments include chemotherapy, radiation therapy, targeted therapy, and immunotherapy. Palliative procedures like ERCP with stent placement are routinely performed to relieve bile duct blockages, manage symptoms, and prevent complications like infection.
Does Medicare cover treatment for bile duct cancer?
Original Medicare (Parts A and B) covers medically necessary services, including hospital stays, doctor visits, surgery, chemotherapy, and radiation. Many patients opt for Medicare Advantage (Part C) plans, which bundle Parts A, B, and usually D (drug coverage), and may offer additional benefits like transportation to appointments or nutrition counseling, which can be invaluable during cancer treatment.
Facing a diagnosis of bile duct cancer is daunting, marked by complex medical decisions and logistical challenges. Building a strong support team, including experienced medical professionals and informed caregivers, is paramount. Equally important is understanding your healthcare coverage to minimize financial stress during treatment. Proactive management, informed by the latest treatment protocols and supported by comprehensive care, offers the best path forward for patients and their families navigating this difficult journey.