Alzheimers Disease Causes: Genetics, Lifestyle, and Risk Factors
Alzheimer’s disease stands as the most common cause of dementia, a progressive brain disorder that erodes memory, thinking skills, and, ultimately, the ability to carry out simple tasks. While the exact trigger for this devastating condition remains elusive, decades of research have illuminated a complex interplay of factors that contribute to its development. Understanding the causes of Alzheimer’s is not just an academic pursuit, it is a crucial step toward identifying risk, developing effective treatments, and, one day, prevention. The prevailing scientific view points to a combination of age-related brain changes, genetic predisposition, environmental influences, and lifestyle factors that, over decades, converge to produce the hallmark symptoms of the disease.
The Core Biological Mechanisms: Plaques and Tangles
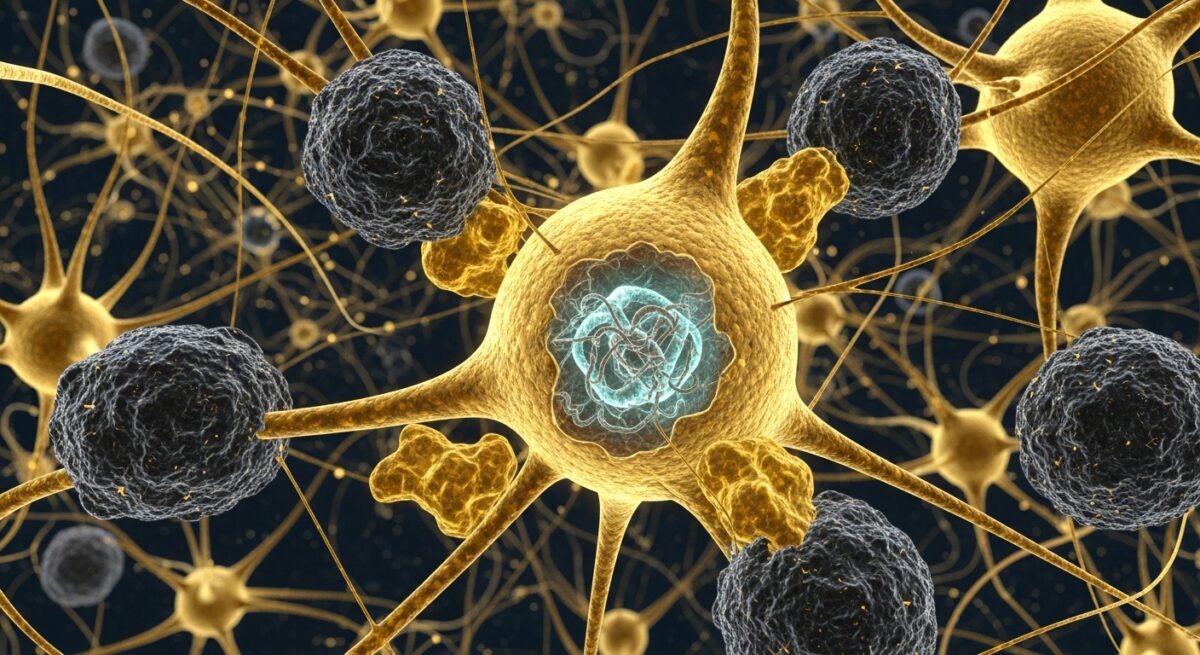
At the heart of Alzheimer’s disease pathology are two abnormal protein structures that disrupt and destroy brain cells: amyloid plaques and neurofibrillary tangles. These are not merely byproducts of the disease, they are central players in its cause and progression. Amyloid plaques are sticky clumps of a protein fragment called beta-amyloid that accumulate in the spaces between nerve cells. In a healthy brain, these protein fragments are broken down and eliminated. In Alzheimer’s, they cluster together, forming hard, insoluble plaques that are thought to interfere with cell-to-cell communication and may trigger an inflammatory response that damages neurons.
Neurofibrillary tangles, on the other hand, occur inside brain cells. They are twisted fibers of a protein called tau. In healthy neurons, tau helps stabilize internal structures called microtubules, which act like tracks to transport nutrients and other essential materials. In Alzheimer’s, tau proteins change shape and organize into tangles. This causes the microtubule system to collapse, crippling the transport system and leading to the failure and death of the cell. The spread of these tau tangles through the brain is closely correlated with the progression of cognitive decline. While these plaques and tangles are the defining features, their precise role as a primary cause or a key consequence is still a subject of intense research, with most experts believing they are directly causative of the neuronal damage.
Genetic Risk Factors: The Role of Inheritance
Genetics play a significant but varied role in the causes of Alzheimer’s disease. Scientists categorize genetic influence into two groups: deterministic genes and risk genes. Deterministic genes are rare and directly cause a disease, guaranteeing that anyone who inherits them will develop the disorder. These genes are responsible for familial Alzheimer’s disease, which accounts for less than 1% of cases and typically has a very early onset (before age 65). Mutations in three genes (APP, PSEN1, and PSEN2) are known to cause this inherited form.
For the vast majority of people with the more common late-onset Alzheimer’s, the genetic picture involves risk genes. These genes increase the likelihood of developing the disease but do not guarantee it. The most well-known and influential genetic risk factor is the apolipoprotein E (APOE) gene on chromosome 19. Everyone inherits some form of APOE, but the APOE ε4 allele variant is the one that increases risk. Inheriting one copy of APOE ε4 from a parent raises risk, while inheriting two copies (one from each parent) raises it even more significantly. However, it is crucial to understand that many people with APOE ε4 never develop Alzheimer’s, and many without it do. This highlights that genetics are just one piece of the puzzle. Other genes are continuously being identified through large genome-wide studies, each contributing a small amount to the overall risk profile.
Modifiable Risk Factors and Lifestyle Influences
Perhaps the most empowering area of research into Alzheimer’s causes involves modifiable risk factors. Unlike our genes, these are elements of our health and environment that we can potentially influence. Strong evidence suggests that the health of the brain is deeply connected to the health of the heart and blood vessels. Conditions that impair cardiovascular health are also implicated in raising Alzheimer’s risk. This is because the brain is highly dependent on a robust blood supply for oxygen and nutrients.
The following lifestyle and health factors are strongly associated with an increased risk of cognitive decline and Alzheimer’s disease:
- Cardiovascular Disease: Hypertension (high blood pressure), high cholesterol, atherosclerosis (hardening of the arteries), and stroke can damage blood vessels in the brain, reducing its efficiency and resilience.
- Diabetes: Type 2 diabetes, especially when poorly managed, impairs the body’s ability to use insulin and can lead to high blood sugar, which is damaging to brain vessels and cells.
- Physical Inactivity: A sedentary lifestyle is linked to a higher risk of Alzheimer’s. Regular physical activity promotes healthy blood flow and is associated with greater brain volume.
- Poor Diet: Diets high in saturated fats, sugar, and processed foods and low in fruits, vegetables, and whole grains may contribute to brain inflammation and vascular damage.
- Smoking: Smoking exposes the brain to oxidative stress and inflammation, accelerating damage to cells and blood vessels.
- Excessive Alcohol Consumption: Heavy, long-term alcohol use is a major risk factor for dementia and can cause direct neurological damage.
- Social Isolation and Cognitive Inactivity: A lack of social engagement and mentally stimulating activities is linked to a higher risk. An intellectually and socially active life may help build cognitive reserve.
Addressing these factors through mid-life and beyond is considered a key strategy for reducing population-level risk. It is important to view Alzheimer’s not as an inevitable consequence of aging, but as a condition whose risk can be modulated by lifelong habits. For a deeper look at how the disease progresses after it begins, our resource on understanding the seven stages of Alzheimers disease outlines the clinical trajectory.
The Impact of Age, Head Trauma, and Other Contributors
The greatest known risk factor for Alzheimer’s disease is advancing age. The likelihood of developing the condition doubles approximately every five years after age 65. This is largely due to the cumulative effect of other risk factors over time, combined with age-related cellular changes that make the brain more vulnerable. These include reduced energy production in cells, increased inflammation, and a diminished capacity for repair. However, Alzheimer’s is not a normal part of aging, it is a specific disease process.
Serious head trauma, particularly incidents involving loss of consciousness, has been clearly linked to a greater risk of dementia later in life. This is believed to be due to the triggering of abnormal tau protein spread, similar to what is seen in chronic traumatic encephalopathy (CTE) found in some athletes. Other potential contributors being studied include chronic, low-level exposure to certain environmental toxins, the role of the gut microbiome, persistent viral infections (like herpes simplex), and prolonged periods of severe stress or depression. The research in these areas is ongoing, aiming to clarify whether they are direct causes or contributing factors that accelerate an underlying process.
Frequently Asked Questions
Can Alzheimer’s disease be prevented?
Currently, there is no proven way to prevent Alzheimer’s. However, a strong body of evidence suggests that managing modifiable risk factors, particularly those related to heart health (like hypertension, diabetes, and obesity), through a healthy diet, regular exercise, not smoking, and controlling alcohol intake, can significantly reduce your overall risk of cognitive decline and dementia.
Is Alzheimer’s disease hereditary?
In most cases, it is not directly inherited in a simple pattern. The rare early-onset familial form is strongly hereditary. For the common late-onset form, having a first-degree relative (parent or sibling) with Alzheimer’s increases your risk, but it does not mean you will definitely develop it. It indicates a combination of shared genetic and environmental factors.
What is the difference between a cause and a risk factor?
A cause is an event or condition that directly produces a disease. A risk factor increases the likelihood of developing the disease but is not sufficient to cause it by itself. For Alzheimer’s, the direct biological cause is the accumulation of plaques and tangles leading to cell death. Risk factors like age, genetics, and poor cardiovascular health create conditions that make this pathological process more likely to occur or progress faster.
Do supplements help prevent Alzheimer’s?
No supplement has been conclusively proven to prevent Alzheimer’s. While some studies have shown associations between certain diets (like the Mediterranean diet) and lower risk, trials for specific supplements like vitamin E, ginkgo biloba, or omega-3s have generally yielded inconsistent or negative results. It is best to focus on obtaining nutrients from a balanced diet and discuss any supplements with a doctor.
If I have memory lapses, does it mean I have Alzheimer’s?
Not necessarily. Occasional memory lapses are a normal part of aging and can also be caused by stress, fatigue, medication side effects, or other medical conditions. The memory loss associated with Alzheimer’s is persistent and progressive, worsening over time and severe enough to disrupt daily life and independent function.
Understanding the multifaceted causes of Alzheimer’s disease demystifies the condition and shifts the narrative from one of passive inevitability to one of informed awareness. While we cannot control our age or genetics, the growing emphasis on modifiable risk factors offers a powerful avenue for public health and personal action. Continued research into the complex interplay between our biology, our behaviors, and our environment holds the key to more effective treatments and, ultimately, the goal of preventing this disease for future generations.
Call 📞833-203-6742 or visit Schedule a Screening to schedule a screening or discuss any persistent symptoms with your healthcare provider.