Can You Have AIDS Without HIV? Clearing Common Myths
The question, ‘can you have AIDS without HIV,’ often arises from confusion about the relationship between HIV infection, immune system damage, and the clinical diagnosis of AIDS. At the heart of this inquiry lies a fundamental misunderstanding of the disease’s progression, which can lead to significant anxiety or misinformation. This article will clarify the crucial medical definitions, explore conditions that can mimic AIDS symptoms, and explain why HIV is the established, non-negotiable cause of acquired immunodeficiency syndrome. Understanding this distinction is vital for personal health management and for navigating coverage options, including how Medicare and other health plans support HIV screening and chronic care.
The Definitive Link Between HIV and AIDS
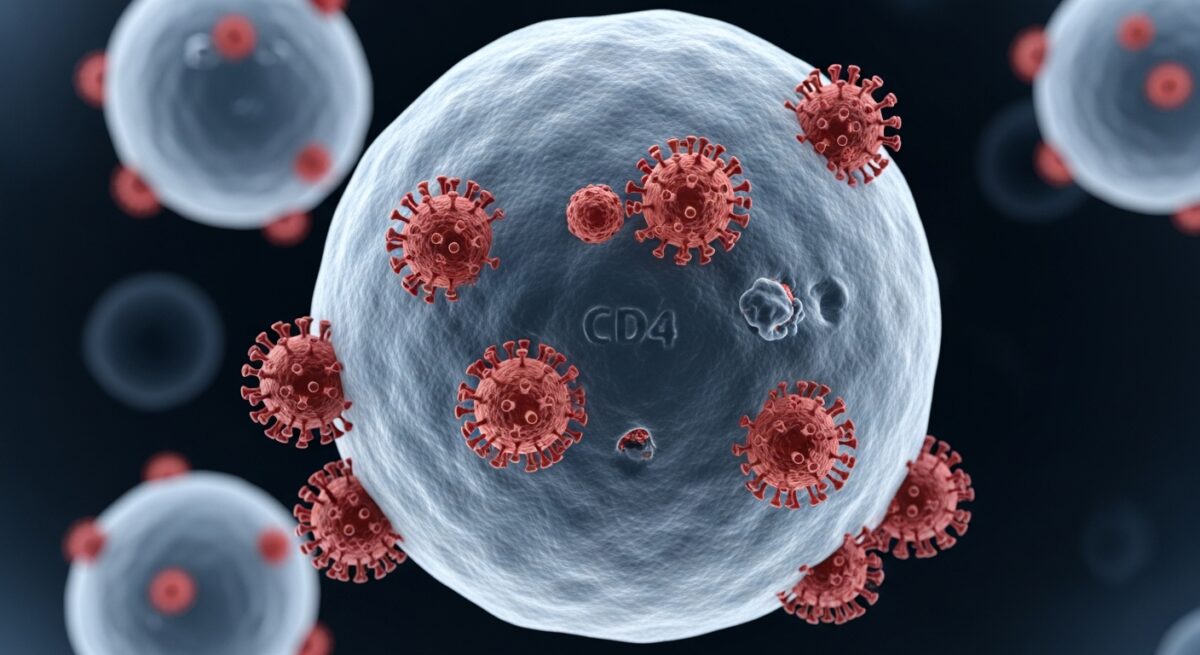
To address the core question, one must first understand the clear medical definitions. Human Immunodeficiency Virus (HIV) is a retrovirus that attacks the body’s CD4 cells (T-cells), which are crucial for a healthy immune system. When left untreated, HIV replicates and gradually depletes these cells, weakening the body’s ability to fight off infections and diseases. Acquired Immunodeficiency Syndrome (AIDS) is not a separate disease but the final, most severe stage of HIV infection. It is diagnosed when the immune system is so badly damaged that specific opportunistic infections or cancers appear, or when a person’s CD4 cell count falls below 200 cells per cubic millimeter of blood. The path is unequivocal: a person contracts HIV, the virus replicates and damages the immune system over time, and without effective treatment, this can lead to an AIDS diagnosis. Therefore, the straightforward answer is no, you cannot have AIDS without first having an HIV infection. The very definition of AIDS is rooted in the damage caused by the HIV virus.
This established causality is backed by decades of overwhelming scientific evidence from virology, epidemiology, and clinical medicine. The discovery of HIV in the 1980s provided the missing link to understanding the mysterious immune collapse seen in AIDS patients. Modern antiretroviral therapy (ART) further proves the connection: by suppressing HIV replication, ART halts immune system decline, prevents the progression to AIDS, and allows many with AIDS to regain a healthy immune status. This successful intervention demonstrates that targeting HIV directly prevents and reverses the conditions that define AIDS. For individuals navigating a new diagnosis, understanding your Medicare coverage for prescription drugs and specialist care is essential to accessing these life-saving treatments.
Conditions That Can Mimic AIDS Symptoms
While AIDS requires an underlying HIV infection, several other medical conditions can cause similar symptoms of a weakened immune system or lead to opportunistic infections. This overlap in symptoms is likely where much of the confusion originates. It is critical to differentiate these conditions from true AIDS, as their causes and treatments are entirely different. A thorough medical evaluation, including a definitive HIV test, is necessary for an accurate diagnosis.
One significant category is primary immunodeficiency disorders (PIDDs). Unlike AIDS, which is ‘acquired’ later in life, PIDDs are typically genetic disorders present from birth that impair the immune system. Examples include Severe Combined Immunodeficiency (SCID) and Common Variable Immunodeficiency (CVID). People with these conditions may suffer from recurrent, severe infections similar to those seen in AIDS, but they have never been exposed to HIV. Their condition stems from an inherent genetic flaw, not a viral infection.
Other conditions that can lead to compromised immunity include certain cancers, such as leukemia and lymphoma, which directly affect bone marrow and blood cells. Advanced autoimmune diseases and their treatments (like high-dose corticosteroids or chemotherapy) can also suppress immune function. Furthermore, severe malnutrition can devastate the immune system’s ability to function, leading to vulnerability to infections. It is important to note that while Medicare covers diagnostic testing for many of these conditions, a specific HIV test is the only way to rule out HIV as the cause of immune deficiency. Our resource on HIV screening details the importance and coverage of this vital test.
The Critical Importance of Accurate HIV Testing
Given the absolute link between HIV and AIDS, accurate and timely HIV testing is the cornerstone of diagnosis and prevention. Modern HIV tests are highly sensitive and specific, and they can detect the virus within weeks of exposure. A negative result from a test taken at the appropriate time reliably rules out HIV infection and, by extension, the possibility of having AIDS caused by HIV. For those who are eligible, understanding your Medicare costs and coverage for preventive services like HIV screening is a key part of proactive health management.
The testing process typically begins with a rapid antibody/antigen test, which can provide results in minutes. A positive result on this initial test is always followed by a confirmatory test to eliminate any chance of a false positive. It is this confirmatory testing that provides a definitive diagnosis. Avoiding testing due to fear or misinformation is dangerous, as early diagnosis and treatment with ART allow people with HIV to live long, healthy lives and virtually eliminate the risk of progressing to AIDS or transmitting the virus to others. Regular screening is recommended for all adults as part of routine healthcare, and it is a covered preventive service under Medicare Part B and most insurance plans.
n
Navigating Treatment and Medicare Coverage
For individuals diagnosed with HIV, early and consistent treatment is the key to preventing AIDS. Antiretroviral therapy (ART) involves taking a combination of HIV medicines daily. This treatment suppresses the viral load to an undetectable level, protects the immune system, and prevents disease progression. Managing HIV is now akin to managing other chronic conditions, requiring regular doctor visits, lab tests, and medication adherence.
Medicare provides essential coverage for people with HIV. Medicare Part B covers outpatient care, including doctor visits, lab tests (like CD4 and viral load monitoring), and preventive services. Medicare Part D covers prescription drugs, which includes the antiretroviral medications crucial for treatment. Some individuals may opt for a Medicare Advantage (Part C) plan, which bundles Part A, Part B, and usually Part D, often with additional benefits. It’s vital to review plan formularies to ensure HIV medications are covered. For those with limited income and resources, programs like the Medicare Part D Extra Help program and state Medicaid can assist with out-of-pocket costs. For more on coordinating benefits, see our guide on if you have Medicare and Medicaid which is primary.
Frequently Asked Questions
Can a person have a weakened immune system without HIV?
Yes, absolutely. Many conditions, such as genetic disorders (primary immunodeficiencies), certain cancers, autoimmune disease treatments, and severe malnutrition, can cause a weakened immune system. However, this is not AIDS unless it is specifically caused by the HIV virus.
Are there false-positive AIDS diagnoses?
AIDS is a clinical diagnosis based on specific criteria (low CD4 count or certain opportunistic infections) in a person with HIV. A false HIV test result could theoretically lead to an incorrect assumption of AIDS risk. This is why any positive HIV screening test is rigorously confirmed with more specific testing before a diagnosis is given.
If my HIV is undetectable, do I still have AIDS?
If you were previously diagnosed with AIDS but your HIV treatment has successfully rebuilt your CD4 count above 200 and you are free of opportunistic infections, you are no longer considered to have an AIDS diagnosis. You are described as a person living with HIV with a restored immune system, thanks to effective therapy.
How does Medicare help with HIV prevention and care?
Medicare Part B covers annual HIV screening for people aged 15-65 and for those at high risk outside this age range. It also covers necessary counseling. For those diagnosed, Medicare covers doctor visits, lab monitoring, and, through Part D or Medicare Advantage, the antiretroviral medications that are the foundation of treatment.
Understanding the unequivocal link between HIV and AIDS dispels a common myth and underscores the importance of prevention, testing, and treatment. You cannot have AIDS without HIV. Recognizing conditions that mimic its symptoms highlights the need for professional medical diagnosis. With modern medicine, an HIV diagnosis is a manageable chronic condition, not an inevitable path to AIDS. Accessing healthcare coverage, such as the preventive screenings and treatment options available through Medicare, is a critical step in maintaining long-term health and well-being for all individuals, regardless of their HIV status.